As warming temperatures make many parts of the world increasingly hospitable to mosquitoes, the risk for dangerous tropical illnesses, such as dengue infection and chikungunya, is expected to spread.
In the face of this growing threat, a new study by Stanford researchers and their Kenyan colleagues sheds light on the factors that put communities at risk for these illnesses—including the presence of trash. With this knowledge, researchers say, communities can better protect themselves from infection.
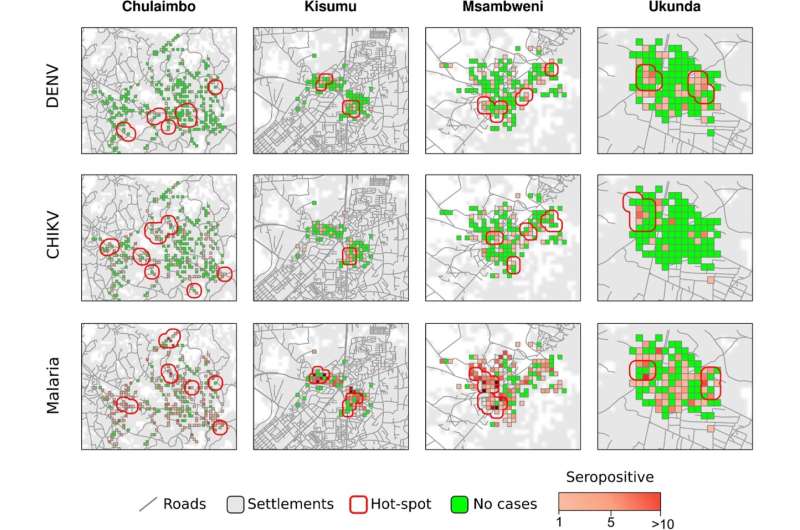
The first-of-its-kind study followed a cohort of 3,521 children in western and coastal Kenya from 2014-2018, testing them for evidence of three potentially deadly, mosquito-borne illnesses: dengue, chikungunya, and malaria. Researchers followed children because it was easier to understand when and where infections occurred in this younger cohort.
By mapping the infections and comparing them with demographic data they gathered, researchers found overlapping hot spots for all three diseases across multiple years. The hot spots were associated with the presence of litter near homes, crowded living arrangements, and relatively greater wealth.
The trash-disease connection
The study, published in BMC Infectious Diseases, adds to a growing body of research that finds strong links between plastic trash and mosquito-borne illness. With formal trash collection still a burgeoning trade in Kenya, many households instead manage their waste by storing it outside their homes and eventually burning it. Plastic containers and rubber tires can hold water that pools during heavy rains, making an ideal breeding ground for mosquitoes.
“These findings underscore our growing concerns over the risks that trash, particularly plastic waste, poses to human health,” said senior author Desiree LaBeaud, MD, a professor of pediatric infectious diseases and global health faculty fellow at the Stanford Center for Innovation in Global Health. “Empowering people to clean up trash from their communities is a clear win-win for human and environmental health.”
Exploring under-studied diseases
The study evolved from the researchers’ desire to better understand the prevalence of two mosquito-borne illnesses, dengue and chikungunya. Like malaria, these diseases are spread by mosquito bites and cause high fever and joint pain. While the symptoms are often mild to moderate, dengue and chikungunya infections can become severe, even deadly.
Despite this, there is little awareness or testing capacity to promptly diagnose dengue and chikungunya in Kenya. Researchers suspected that dengue and chikungunya were in fact responsible for many of the infections attributed to malaria, which is often assumed to be the cause of patients’ fevers.
“When a patient comes into the clinic with a fever, it’s important to be able to make an accurate diagnosis,” said Aslam Khan, DO, a clinical assistant professor of pediatric infectious diseases, global health faculty fellow, and lead author of the study. “Without the ability to make an accurate diagnosis, we risk over-prescribing ineffective antimalarials or antibiotics, building antibiotic resistance.”
Common hotspots offer win-win solutions
Overall, 9.8% of children in the study had antibodies in their bloodstream indicating a prior infection for chikungunya and 5.5% were for dengue. Of children who were tested, 39.1% were positive for malaria. The researchers were surprised to find hot spots where the risk for all three diseases was higher.
“These common hot spots suggest that both the built environment and social factors can significantly influence the risk of various mosquito-borne infections,” said Khan.
The study also indicated that malaria risk had the strongest association with litter.
Currently, most of Kenya’s prevention measures are targeted toward the Anopheles species of mosquito that causes malaria, which bites at night. For instance, bed netting is a common malaria intervention that does little to prevent dengue or chikungunya, which are spread by a mosquito active during the day. This study, Khan said, revealed measures that could be effective at targeting both mosquitoes, including using window screens, eliminating open water containers, and removing trash from around homes.
LaBeaud noted that the link between trash and malaria was particularly interesting given that a new malaria vector, Anopheles stephensi, was recently discovered for the first time in northern Kenya. Like the Aedes aegypti mosquito that spreads dengue and chikungunya, Anopheles stephensi has adapted to breeding in human-made water containers in urban areas. LaBeaud’s team is exploring future studies to see if this mosquito is involved in malaria transmission where they are working.
HERI Kenya, a nonprofit organization co-founded by LaBeaud in response to her findings about the connection between plastic trash and disease, is working to empower and educate Kenyan communities to clean up and recycle plastic trash.
Doing so offers many additional health and economic benefits to the community, including reduced pollution, fewer toxic fumes from burning waste, and new income opportunities for recyclers, LaBeaud said.
Khan hopes the study will also help support increased awareness and testing capacity for dengue and chikungunya. He said he has already seen a shift in awareness on the part of the health workers who helped with the study. “Our community team members are now very cognizant that dengue and chikungunya could be the culprits when they see a sick patient,” he said.
More information:
Aslam Khan et al, Spatiotemporal overlapping of dengue, chikungunya, and malaria infections in children in Kenya, BMC Infectious Diseases (2023). DOI: 10.1186/s12879-023-08157-4
Journal information:
BMC Infectious Diseases
Source: Read Full Article