MUSC researchers have identified a novel biomarker that could change the way sepsis is approached and treated. Sepsis, the leading cause of death in intensive care units, is the body’s extreme response to an infection and can lead to organ damage and failure.
In a recent study in Frontiers in Immunology, the researchers report that the severity of sepsis could be predicted by the contents of membranous structures known as extracellular vesicles, or EVs, that are shed by cells into the bloodstream. Based on sepsis severity, treatment protocols could then be tailored to individual patients and reduce the mortality rate and organ failure associated with severe sepsis.
“In sepsis, the major problem is organ dysfunction,” said Hongkuan Fan, Ph.D., associate professor in the College of Medicine, who studies vascular dysfunction in sepsis.
Acute kidney injury (AKI) and acute respiratory distress syndrome (ARDS) are complications of severe sepsis that arise when the blood vessels become leaky and major organs are unable to get the required amount of oxygen and nutrients. AKI usually results in a very sudden reduction in kidney function, making it difficult for the kidneys to filter waste products from the blood. ARDS commonly causes respiratory failure in critically ill patients, like those in the ICU, making it difficult for them to breathe.
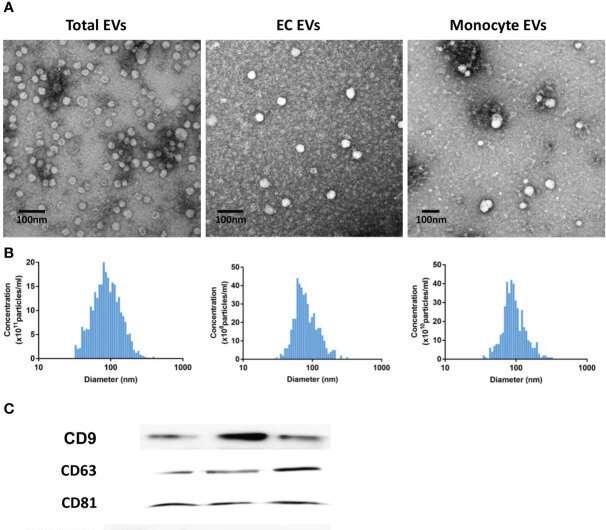
The MUSC team studied the content of EVs because they are produced in high numbers by white blood cells and platelets during sepsis. EVs carry proteins and RNA throughout the body that can modify the function of other cells that pick them up. When these modified cells penetrate through the walls of leaky blood vessels, organ damage can occur. The complex and intricate functions of the body work to maintain homeostasis, or balance, and this balance can be easily disrupted by minor changes like an infection.
“Normal blood vessel walls could protect tissues; however, in a disease condition such as sepsis, larger molecules and cells can pass through this blood vessel wall, which can induce inflammation and will worsen the situation during sepsis,” said Pengfei Li, Ph.D., lead author and staff scientist in the Department of Pathology and Laboratory Medicine.
The body relies on immune cells, a large group of cells that defend it from invaders, to clear an infection. However, sepsis severity cannot be determined by tracking just immune cells. Fan and Li believe that EV content could better group patients, because EVs are released from all types of cells, not just immune cells. As such, they could provide more information about possible organ malfunction or damage occurring throughout the body.
With statistical support from the South Carolina Clinical & Translational Research (SCTR) Institute, the researchers analyzed the content of EVs. They found that EVs from septic patients contained higher levels of certain enzymes and lower levels of one specific RNA molecule when compared with critically ill nonseptic patients and healthy patients from MUSC.
Patients with circulating EVs that caused cell injury were more likely to develop ARDS, and EVs that showed a decline in specific RNA levels were also associated with increased mortality from ARDS and AKI.
“While further validation studies and larger cohorts of septic patients are necessary,” said Li, “EV content could be a dynamic marker for sepsis.”
Many hurdles must be cleared before these biomarkers are used in the clinic, but certain factors could speed progress. For EVs, that technology already exists. A simple blood test known as a liquid biopsy could be used to collect and analyze EVs and the changes that occur in their contents in a patient with sepsis. The MUSC research team hopes that by studying the proteins and RNA found in the EVs, sepsis severity can be predicted, allowing treatment to be tailored to the individual patient.
More information:
Pengfei Li et al, Circulating extracellular vesicles are associated with the clinical outcomes of sepsis, Frontiers in Immunology (2023). DOI: 10.3389/fimmu.2023.1150564
Journal information:
Frontiers in Immunology
Source: Read Full Article
