A research team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered that exosomes derived from γδ-T cells (γδ-T-Exos) synergized with radiotherapy can control nasopharyngeal carcinoma (NPC) by overcoming the radioresistance of NPC cancer stem cells (CSCs) and preserve their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. This study provides a proof of concept for a novel and potent strategy by combining γδ-T-Exos with radiotherapy in the control of NPC. The findings have been published in the Journal for Immunotherapy of Cancer.
Nasopharyngeal carcinoma (NPC) is one of the most aggressive Epstein-Barr virus (EBV)-associated tumors, which are very prevalent in East Asia, including Hong Kong. Radiotherapy is the first-line treatment for NPC, but its therapeutic efficacy is poor in some patients due to radioresistance. Adoptive T cell-based immunotherapy has also shown promise to control NPC; however, its anti-tumor efficacy may be attenuated by an immunosuppressive tumor microenvironment. Exosomes are endosome-originated small extracellular vesicles that mediate intercellular communication. Compared with cell-based therapy, cell-free exosomes have advantages with higher safety, easier storage and lower costs. In a previous study, researchers have demonstrated that γδ-T-Exos could effectively control the progression of EBV-associated tumors. However, it remains unknown whether γδ-T-Exos have synergistic effect with radiotherapy and preserve their anti-tumor activities against NPC in an immunosuppressive tumor microenvironment.
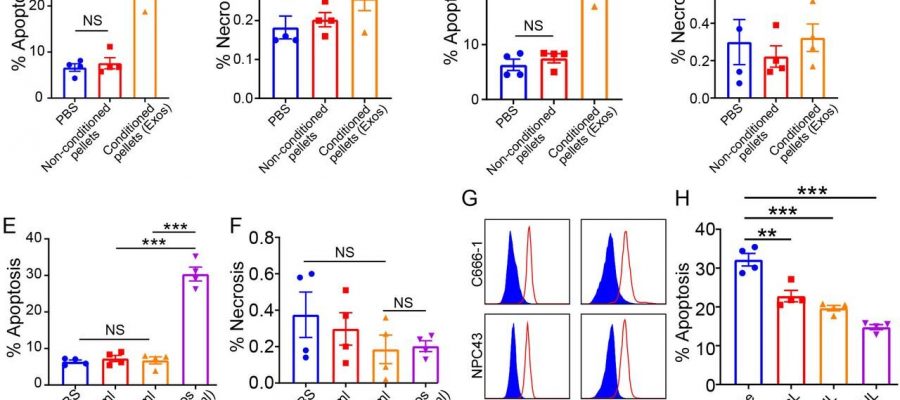
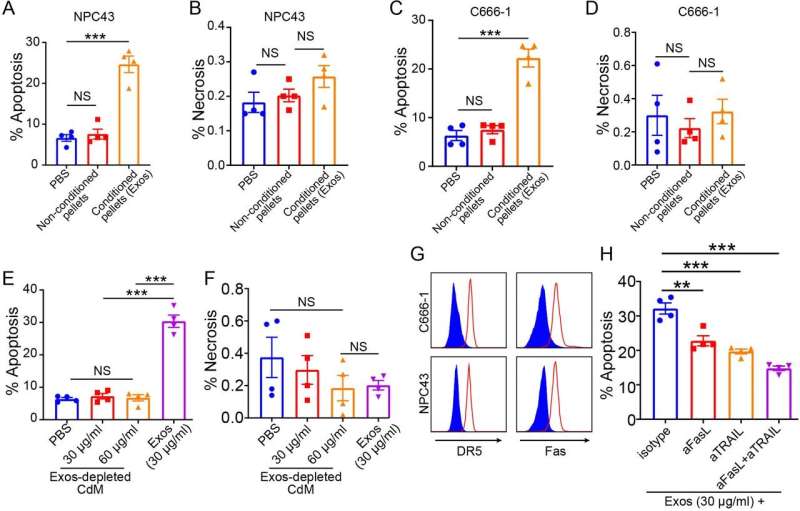
The research team found that γδ-T-Exos not only effectively interacted with NPC cells and induced tumor cell death in vitro, which was mainly mediated by Fas/Fas ligand (FasL) and death receptor 5 (DR5)/tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) pathways, but also controlled NPC tumor growth and prolonged tumor-bearing mice survival in vivo. Furthermore, γδ-T-Exos selectively targeted the radioresistant CD44+/highCSCs and induced profound cell apoptosis. The combination of γδ-T-Exos with radiotherapy overcame the radioresistance of CD44+/highNPC cells and significantly improved its therapeutic efficacy against NPC in vitro and in vivo. In addition, γδ-T-Exos promoted T-cell migration into NPC tumors by upregulating CCR5 on T cells that were chemoattracted by CCR5 ligands in the NPC tumor microenvironment. Although NPC tumor cells secreted abundant tumor growth factor beta (TGF-β) to suppress T- cell responses, γδ-T-Exos preserved their direct anti-tumor activities and overcame the immunosuppressive NPC microenvironment to amplify T-cell anti-tumor immunity.
“Our study first provides a strong pre-clinical proof of concept using a novel therapeutic strategy by combining γδ-T-Exos with radiotherapy to treat NPC. γδ-T-Exos can effectively interact with and kill both EBV positive and negative NPC cells. More importantly, γδ-T-Exos can eradicate radioresistant NPC CSCs and preserve their tumor-killing and T cell-promoting activities in the immunosuppressive NPC microenvironment. Therefore, combination of radiotherapy with γδ-T- Exos has great potential in the treatment of NPC, which will be highly beneficial to the clinical application of this approach,” said Professor Tu Wenwei of the Department of Pediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed, who led the research.
Significance of the study
Source: Read Full Article