Many people commonly consume fiber-enriched foods to promote weight loss and prevent chronic diseases such as diabetes and cancer.
However, in some individuals—particularly those with a silent vascular deformity—consumption of highly refined fiber may increase the risk of liver cancer, new research from The University of Toledo has found.
The discovery, detailed in a paper published in the journal Gastroenterology, builds on UToledo’s growing area of research expertise that our gut plays an underappreciated role in the origin of disease.
“We have worked for a long time on this idea that all diseases start from the gut,” said Dr. Matam Vijay-Kumar, a professor in the Department of Physiology and Pharmacology in the College of Medicine and Life Sciences and the paper’s senior author. “This study is a notable advancement of that concept. It also provides clues that may help identify individuals at a higher risk for liver cancer and potentially enable us to lower that risk with simple dietary modifications.”
Expanding research
Four years ago, Vijay-Kumar’s team published a major paper in the journal Cell that found a high percentage of mice with immune system defects developed liver cancer after being fed a diet fortified with inulin.
A refined, plant-based fermentable fiber, inulin is available in supermarkets as a health-promoting prebiotic. It is also a common ingredient of processed foods.
While inulin promotes metabolic health in most who consume it, Vijay-Kumar and colleagues discovered that about one in 10 standard, seemingly healthy lab mice developed liver cancer following consumption of the inulin-containing diet.
“That was very surprising, given how rarely liver cancer is observed in mice,” said Vijay-Kumar, who is also director of the UToledo Microbiome Consortium. “The findings raised real questions about the potential risks of certain refined fibers, but only now do we understand why the mice were developing such aggressive cancer.”
The new study offers a clear explanation—and may have implications that go beyond laboratory animals.
A missing link
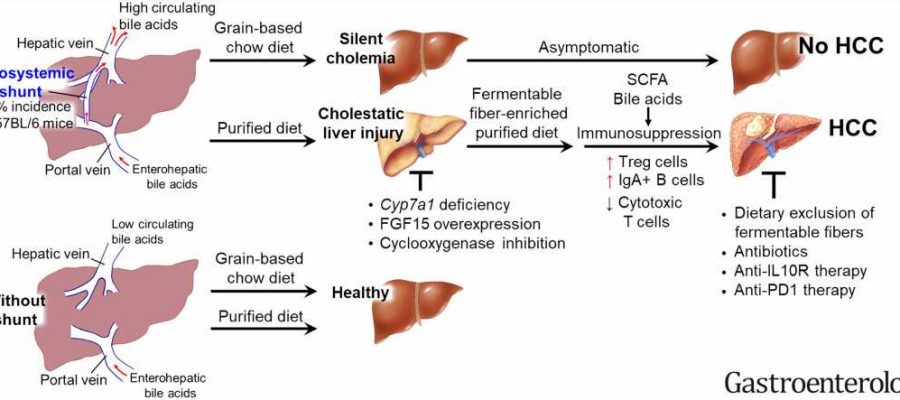
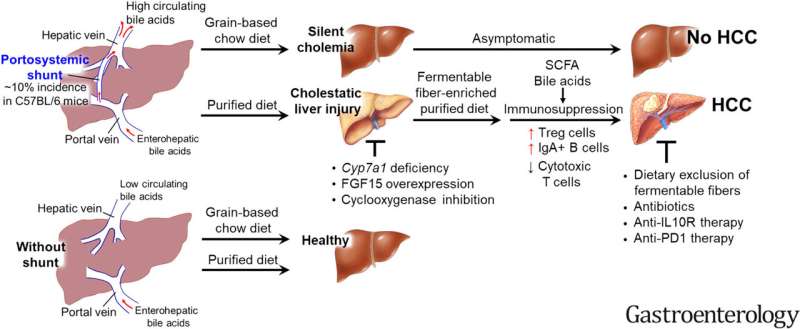
As the team furthered its investigation, the researchers discovered all mice that developed malignant tumors had high concentrations of bile acids in their blood caused by a previously unnoticed congenital defect called a portosystemic shunt.
Normally, blood leaving the intestines goes into the liver where it is filtered before returning to the rest of the body. When a portosystemic shunt is present, blood from the gut is detoured away from the liver and back into the body’s general blood supply.
The vascular defect also allows the liver to continuously synthesize bile acids. Those bile acids eventually spill over and enter circulation instead of going into the gut.
Blood that’s diverted away from the liver contains high levels of microbial products that can stimulate the immune system and cause inflammation.
To check that inflammation, which can be damaging to the liver, the mice react by developing a compensatory anti-inflammatory response that dampens the immune response and reduces their ability to detect and kill cancer cells.
While all mice with excess bile acids in their blood were predisposed to liver injury, only those fed inulin progressed to hepatocellular carcinoma, a deadly primary liver cancer.
Remarkably, 100% of the mice with high bile acids in their blood went on to develop cancer when fed inulin. None of the mice with low bile acids developed cancer when fed the same diet.
“Dietary inulin is good in subduing inflammation, but it can be subverted into causing immunosuppression, which is not good for the liver,” said Dr. Beng San Yeoh, a postdoctoral fellow and the new paper’s first author.
Dr. Bina Joe, Distinguished University Professor and chair of the Department of Physiology and Pharmacology, and a co-author of the study, said the high-impact publication demonstrates the pioneering research being done at UToledo.
“The role of the gut and gut bacteria in health and disease is an exciting and important area of research, and our team is providing new insights on the leading edge of this field,” she said.
Implications
Beyond the laboratory, UToledo’s research could provide insight that might help clinicians identify people who are at higher risk of liver cancer years in advance of any tumors forming.
Portosystemic shunts in humans are relatively rare—the documented incidence is only one in 30,000 people at birth. However, given that they generally cause no noticeable symptoms, the true incidence may be many times greater. Portosystemic shunting also commonly develops following liver cirrhosis.
Theorizing that high bile acid levels might serve as a viable marker for liver cancer risk, Vijay-Kumar’s team tested bile acid levels in serum samples collected between 1985 and 1988 as part of a large-scale cancer prevention study.
In the 224 men who went on to develop liver cancer, their baseline blood bile acid levels were twice as high as men who did not develop liver cancer. A statistical analysis also found individuals with the highest blood bile acid levels had a more than four-fold increase in the risk of liver cancer.
The research team also sought to examine the relationship between fiber consumption, bile acid levels and liver cancer in humans.
While existing epidemiological studies don’t differentiate between soluble and non-soluble fiber, researchers could look at fiber consumption in concert with blood bile acids.
There are two basic types of naturally occurring dietary fiber, soluble and insoluble. Soluble fibers are fermented by gut bacteria into short-chain fatty acids. Insoluble fibers pass through the digestive system unchanged.
Intriguingly, researchers found high total fiber intake reduced the risk of liver cancer by 29% in those whose serum bile acid levels were in the lowest quartile of their sample.
However, in men whose blood bile acid levels placed them in the top quarter of the sample, high fiber intake conferred a 40% increased risk of liver cancer.
Taken together, Yeoh and Vijay-Kumar say the findings suggest both the need for regular blood bile acid level testing and a cautious approach to fiber intake in individuals who know they have higher-than-normal levels of bile acids in their blood.
“Serum bile acids can be measured by a simple blood test developed over 50 years ago. However, the test is usually only performed in some pregnant women,” Vijay-Kumar said. “Based on our findings, we believe this simple blood test should be incorporated into the screening measurements that are routinely performed to monitor health.”
And while the researchers are not arguing broadly against the health-promoting benefits of fiber, they are urging attention to what kind of fiber certain individuals eat, underscoring the importance of personalized nutrition.
Source: Read Full Article