New research hints at the possibility that cerebral amyloid angiopathy (CAA), a cause of spontaneous brain hemorrhage, can be transmitted via blood transfusion, raising the risk for spontaneous intracerebral hemorrhage (ICH) in transfusion recipients.
In an exploratory analysis, receiving red blood cell transfusions from donors who later developed multiple spontaneous ICHs, and were assumed to have CAA, were at a significantly increased risk of developing spontaneous ICH themselves.
“This may suggest a transfusion-transmissible agent associated with some types of spontaneous ICH, although the findings may be susceptible to selection bias and residual confounding, and further research is needed to investigate if transfusion transmission of CAA might explain this association,” the investigators note.
“We do not think that the findings motivate a change in practice, and we should not let these results discourage otherwise indicated blood transfusion,” lead author Jingcheng Zhao, MD, PhD, with Karolinska University Hospital Solna in Stockholm, Sweden, told Medscape Medical News.
The study was published online September 12 in the Journal of the American Medical Association.
Novel Finding
Recent evidence suggests that CAA exhibits “prion-like” transmissivity, with reports of transmission through cadaveric pituitary hormone contaminated with amyloid-beta and tau protein, dura mater grafts and possibly neurosurgical instruments.
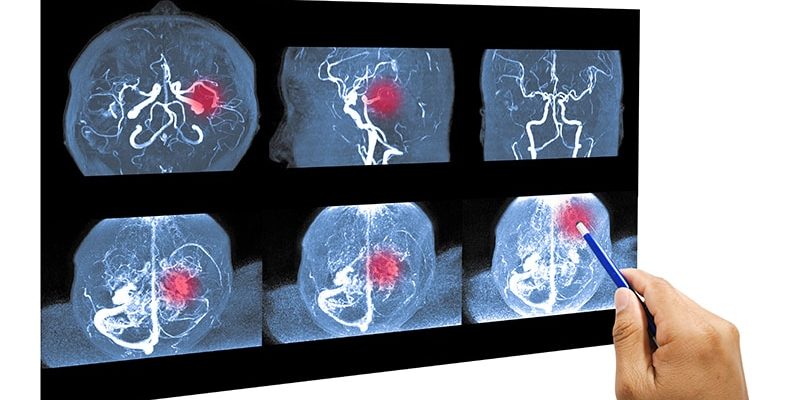
CAA, which is characterized by the deposition of amyloid protein in the brain, is the second most common cause of spontaneous ICH.
The researchers hypothesized that transfusion transmission of CAA may manifest through an increased risk for spontaneous ICH among transfusion recipients given blood from a donor with spontaneous ICH.
To explore this hypothesis, they analyzed national registry data from Sweden and Denmark for ICH in recipients of red blood cell transfusion from donors who themselves had ICH over the years after their blood donations, with the assumption that donors with two or more ICHs would likely have CAA.
The cohort included nearly 760,000 individuals in Sweden (median age, 65 years; 59% women) and 330,000 in Denmark (median age, 64 years; 58% women), with a median follow-up of 5.8 and 6.1 years, respectively.
Receiving red blood cell transfusions from donors who later developed multiple spontaneous ICHs was associated with a greater than twofold increased risk of developing spontaneous ICH compared with receiving a transfusion from donors without subsequent ICH (hazard ratio [HR] 2.73; P < .001 in the Swedish cohort and HR 2.32; P = .04 in the Danish cohort).
“The observed increased risk of spontaneous ICH associated with receiving a red blood cell transfusion from a donor who later developed multiple spontaneous ICHs, corresponding to a 30-year cumulative incidence difference of 2.3%, is a novel finding,” the researchers write.
There was no increase in post-transfusion ICH risk among recipients whose donors had a single post-blood-donation ICH.
The findings were robust to several of the sensitivity analyses.
A “negative” control analysis of post-transfusion ischemic stroke (instead of ICH) found no increased risk among recipients of blood from donors who had single or multiple ICHs.
This study provides “exploratory evidence of possible transfusion-transmission of a factor that causes ICHs, but more research is needed to confirm and to understand the mechanism,” said Zhao.
The researchers note that they did not directly assess CAA but expect it would be more common among donors who develop multiple spontaneous ICHs, “as CAA-related ICH has been reported to have a 7-fold increase for recurrent ICHs compared with non–CAA-related ICH.”
Worrisome Finding or False Alarm?
In a JAMA editorial , Steven Greenberg, MD, PhD, with the Department of Neurology, Harvard Medical School, Boston, says there are “good reasons to treat the possibility of CAA transmission via blood transfusion seriously — and good reasons to remain skeptical at least for the present.”
“Powerful” arguments in support of the findings include the robust study methodology and the “striking” similarity in results from the two registries, which argues against a chance finding.
Another is the negative control with ischemic stroke as the outcome, which argues against unsuspected confounding-causing associations with all types of stroke, Greenberg notes.
Arguments for remaining “unconvinced” of the association center on the weakness of evidence for a plausible biological mechanism for the finding, he points out.
Another is the short-time course of ICHs after blood transfusion, which is “quite challenging to explain,” Greenberg said. Nearly half of the ICHs among blood recipients occurred within 5 years of transfusion, which is “dramatically” faster than the 30- to 40-year interval reported between neurosurgical exposure to cadaveric tissue and first ICH, he adds.
Another related “mechanistic reservation” is the plausibility that a transmissible species of amyloid-beta could travel from blood to brain in sufficient quantities to trigger advanced CAA or Alzheimer disease pathology, he writes.
He added the current study leaves him “squarely at the corner of anxiety and skepticism.”
With more than 10 million units of blood transfused in the US each year, even a modest increase in risk for future brain hemorrhages or dementia conferred by “an uncommon — but as of now undetectable — donor trait would represent a substantial public health concern,” Greenberg writes.
“From the standpoint of scientific plausibility, however, even this well-conducted analysis is at risk of representing a false alarm,” he cautions.
Looking ahead, Greenberg says one clear direction is independent replication, ideally with datasets in which donor and recipient dementia can be reliably ascertained to assess the possibility of Alzheimer’s disease as well as CAA transmissibility.
“The other challenge is for experimental biologists to consider the alternative possibility of transfusion-related acceleration of downstream steps in the CAA-ICH pathway, such as the vessel remodeling by which amyloid β–laden vessels proceed to rupture and bleed.
“The current study is not yet a reason for alarm, certainly not a reason to avoid otherwise indicated blood transfusion, but it is a strong call for more scientific digging,” Greenberg concludes.
The study was funded by grants from the Karolinska Institute, the Swedish Research Council, and Region Stockholm. Zhao and Greenberg report no relevant financial relationships.
JAMA. Published online September 12, 2023. Abstract, Editorial
For more Medscape Neurology news, join us on Facebook and Twitter
Source: Read Full Article