Pelvic inflammatory disease (usually referred to as PID) represents a complex infection that affects millions of women worldwide. It should be considered as a spectrum of reproductive tract infections, and viewed as a dynamic progressive infection that can rapidly migrate from the cervix to the uterus and involve fallopian tubes and ovaries.
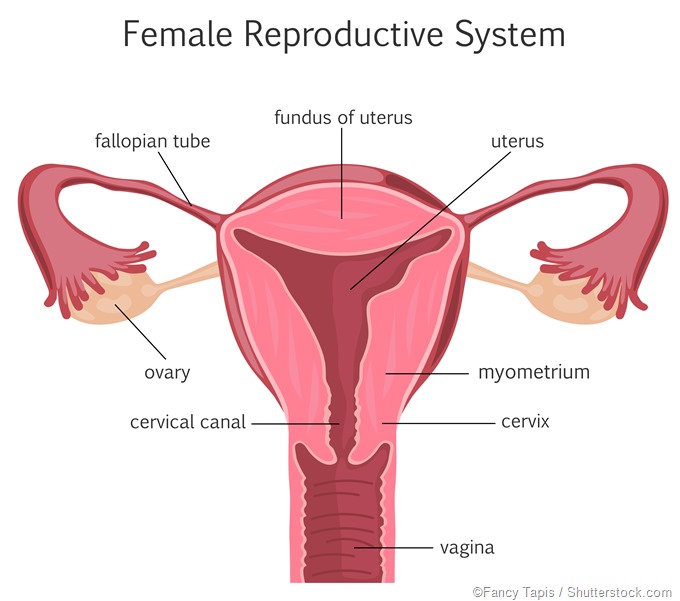
Once the disease has shown a progressive route, it can result in devastating consequences on the reproductive tract and the reproductive capabilities of affected women. The biggest problem is that the disease is often asymptomatic, thus women with this infection are not aware of its presence, nor that their reproductive capability has been jeopardized.
The condition is most often caused by the sexually-transmitted pathogens Chlamydia trachomatis and Neisseria gonorrhoeae. Mycoplasma genitalium and microorganisms associated with bacterial vaginosis also play a prominent role in PID and are increasingly being sought in microbiological evaluations.
In any case, due to potential serious consequences, all key players responsible for the care of women (most notably gynecologists, obstetricians, general practitioners, but also nurses and residents in training) have a major role in the prevention and appropriate treatment of PID.
Epidemiology of pelvic inflammatory disease
As PID is not a reportable disease, it is quite difficult to accurately ascertain the number of women affected by this condition on an annual basis. By analyzing outpatient and hospital discharge codes, the Centers for Disease Control and Prevention (CDC) estimates that more than 750 thousand women experience an episode of acute PID every year.
Furthermore, in the United States, PID is a common cause of visits to the emergency department, with 106 thousand outpatient visits and 60 thousand hospitalizations every year. Financial aspects are substantial as well; therapy costs for each affected women with PID are approximately two thousand USD, which can rise up to six thousand USD if chronic pelvic pain ensues.
Surveillance and early detection would, therefore, be a way forward. Therein lies the problem; there is no simple, cheap, and accurate diagnostic test or PID. Furthermore, there is no single infection as the cause of PID and no pathognomonic (i.e. disease-specific) signs or symptoms, which is further compounded by the fact that routine, large scale diagnostic techniques can hardly reach the female upper genital tract.
Generally, disease rates are two to three times higher among African-American women when compared to Caucasian women, which is consistent with the pronounced racial disparities observed for both gonorrhea and chlamydia. Nevertheless, if we take into account the subjective methods by which PID is usually diagnosed, such data on racial disparity may be inaccurate.
Hospital admission rates may serve as a crude marker of this condition in resource-poor countries, where PID is responsible for 17 to 40 percent of all gynecological hospital admissions in sub-Saharan Africa, up to 37 percent in Southeast Asia, and 3 to 10 percent in India.
Risk factors for developing the condition
At the greatest risk of developing PID are young women with multiple partners; and indeed, most of the cases are seen in women between 15 and 29 years of age. This may be partially due to an immature cervix which predisposes them to the infection with the commonly causative organisms. A previous history of PID also increases the risk of successive episodes.
In the past, intrauterine devices (IUDs) had been considered the main culprits for developing PID. Today it is known that the use of modern IUDs increase the risk by only a margin, which is reduced even more if a woman is tested and (if necessary) treated for sexually-transmitted infections before their insertion.
Refraining from the use of condoms and barrier methods also increases the risk of developing PID. Some studies have also demonstrated a protective effect of combined oral contraceptives. While current research suggests that they do not decrease the incidence of developing PID, it has been shown that they do reduce the severity of the condition.
Sources
- http://sti.bmj.com/content/76/2/80
- http://www.aafp.org/afp/2012/0415/p791.html
- http://www.nejm.org/doi/pdf/10.1056/NEJMra1411426
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3843151/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907941/
- Barash JH, Hillson C, Buchanan E, Suaray M. Pelvic Inflammatory Disease. In: Skolnik NS, Clouse AL, Woodward JA. Sexually Transmitted Diseases: A Practical Guide for Primary Care. Springer Science & Business Media, 2013; pp. 71-84.
Further Reading
- All Pelvic Inflammatory Disease (PID) Content
- Pelvic Inflammatory Disease Clinical Presentation
- Pelvic Inflammatory Disease Diagnosis
- Pelvic Inflammatory Disease Etiology
- Pelvic Inflammatory Disease Management and Prognosis
Last Updated: Feb 27, 2019

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article
