Retinal thickness may be a potential biomarker for predicting disability for patients newly diagnosed with relapsing multiple sclerosis (MS), new research suggests.
Researchers measured retinal thickness using optical coherence tomography (OCT) within 3 months of diagnosis for more than 230 patients with MS and found that thinning of the retina was associated with a more than fourfold increased risk of Expanded Disability Status Scale (EDSS) scores ≥3.0.
The OCT “basically tells you how much nerve layer is left in the glass,” said study investigator Gabriel Bsteh, MD, PhD, Department of Neurology, Medical University of Vienna, Vienna, Austria.
This “could potentially inform treatment strategies, but that is another direction which will be investigated hopefully in the near future,” he added.
However, the imaging technique cannot be used for all patients and is currently not widely available, he noted.
Bsteh presented the results at the Congress of the European Academy of Neurology (EAN) 2023.
Retinal Layers of Interest
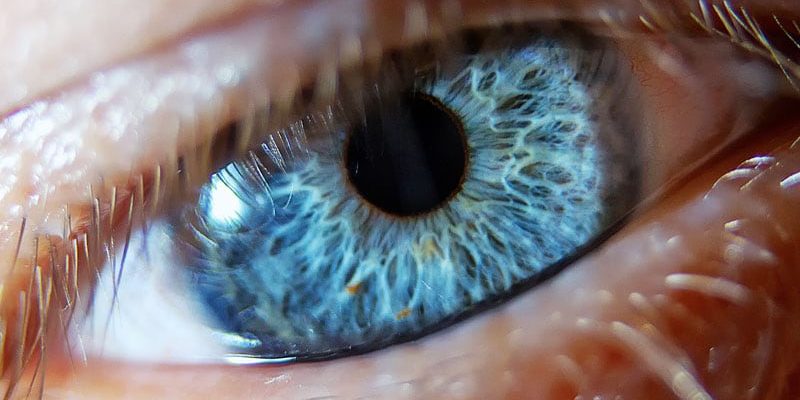
OCT produces images of the retina and measures its thickness, Bsteh explained. Of greatest interest and relevance to patients with MS are two layers ― the peripapillary retinal nerve fiber layer (pRNFL) and the ganglion cell and inner plexiform layer (GCL), which are associated with “future physical and cognitive disability and brain atrophy, and are reliable biomarkers of axonal damage,” he said.
However, he said, what is not yet known is whether the baseline thickness of these two layers independently predicts progression of disability in patients with newly diagnosed disease within the framework of all of the other known risk factors.
To investigate, the team used data from ViennOCTiMS, an ongoing prospective observational cohort study conducted in Vienna and Innsbruck. For the analysis, they included patients newly diagnosed with relapsing MS using the 2017 McDonald criteria.
Study participants were required to undergo a spectral-domain OCT scan within 90 days of diagnosis and within 270 days of symptom onset. They also had to undergo follow-up of at least 12 months.
Among 231 patients included in the study, 74.0 were female, and the mean age was 30.3 years.
Bsteh noted that disease duration was short. There was a median of 45 days between initial diagnosis and the OCT scan. The median number of T2 lesions on MRI was 11, with 59.3% of patients had at least 10 lesions.
At baseline, 13.0% of patients were not receiving drug therapy, although they were advised to do so, said Bsteh. A total of 59.7% of patients received “moderately effective” disease-modifying treatments (DMTs), while 27.3% were treated with “highly effective” DMTs.
Independent Predictors of Disability
To determine the contribution of retinal thickness to the risk of developing EDSS ≥3.0, the researchers conducted a multivariate analysis that accounted for patient age and sex, the type of first relapse, the remission of first relapse symptoms, the presence of oligoclonal bands, the baseline number of T2 lesions, and the use and type of DMT.
After approximately 96 months of follow-up, a pRNFL thickness of ≤88 µm at baseline was associated with a hazard ratio for EDSS ≥3.0, vs a thickness of >88 µm of 4.0 (P < .001), Bsteh reported.
Similarly, a GCL thickness of <77 µm at baseline was associated with a hazard ratio for EDSS ≥3.0 of 5.1 (P < .001).
Subgroup analysis indicated that both measures of retinal thickness were indeed independent predictors of EDSS. Bsteh said, “It was encouraging to see that all the unknown prognostic factor factors performed within the expected framework.”
For example, there was a notable association between the risk of EDSS ≥3 and patient age, as well as with incomplete remission and a greater number of lesions on MRI.
Bsteh said it was also “very encouraging” to find that high-efficacy DMT was associated with a reduced risk of EDSS ≥3.0.
Strengths, Limitations
Turning to the relatively recently described progression independent of relapse activity (PIRA), Bsteh showed that both pRNFL ≤88 µm and GCL <77 µm were significantly associated with the development of PIRA compared to greater thickness, at hazard ratios of 3.1 and 4.1, respectively (P < .001 for both).
Subgroup analysis again supported the independent contribution of retinal thickness to the risk of PIRA and revealed similar associations with known risk factors, although the contribution of highly effective DMT was of borderline significance for this outcome.
Interestingly, neither pRNFL ≤88 µm nor GCL <77 µm was significantly associated with the time to second clinical attack, “which is basically the correlation of the inflammatory activity” in MS, said Bsteh.
This, he continued, “goes back to the basic theory that EDSS, PIRA, and neurodegenerative problems are associated with the OCT but not the degree of inflammatory activity.
“As good as all that sounds, there are of course, some limitations” to the study, Bsteh acknowledged.
The most important limitation is that the changes measured on OCT were “not specific to multiple sclerosis,” and the thickness of the layers “can be influenced by a lot of other factors,” in particular by eye conditions such as glaucoma and diabetes mellitus.
In addition, OCT is not reliable for patients with myopia of more than 4–6 diopters and for those with retinal comorbidities, such as optic drusen. Bsteh also pointed out that automatic segmentation in OCT requires stringent quality control.
However, the “biggest problem for the deployment of OCT in the clinical routine is its lack of availability. It’s not very easy for neurologists to procure an OCT,” said Bsteh.
“You can always create it with your ophthalmologist of trust, but you have to know what you’re looking for,” he added.
Important Research
Commenting on the study, Giancarlo Comi, MD, honorary professor of neurology at the Università Vita Salute San Raffaele and founder and director of the Institute of Experimental Neurology at the Scientific Institute San Raffaele, Milan, Italy, characterized the research as “very, very important and interesting.”
However, he said that he was a “bit surprised” that it showed no association between OCT measures and the second clinical attack, noting that longitudinal research by his team found such an association.
Comi added that the “key point” from the current study is that there was no such association in the early phase of the disease, which suggests that the amount of inflammatory activity “is not so relevant” in determining the degree of damage seen on OCT at that point.
Bsteh said he partially agreed with Comi, adding that “it depends on what you adjust for.
“If we did the same analysis without adjusting for the number of MRI lesions, we would see an association with second clinical attack,” he said. However, he added, the aim of the current study was to determine the independent contribution of retinal thickness, “and that’s why we tried to adjust to everything which was available to us.”
Bsteh also underlined that it was a cross-sectional analysis conducted “very, very early” in the MS disease course, and “so the inflammatory activity did not yet have a chance to influence the thickness on the OCT.”
Had OCT been performed later in the disease course, inflammatory activity might have influenced the findings, but the intention of the study was to use it “as an early marker to try to stratify patients who are at risk, and [those] who are maybe a little less at risk, and inform the treatment strategy.”
Maria Assunta Rocca, MD, associate professor of neurology at Vita-Salute San Raffaele University, and head of the neuroimaging of CNS White Matter Unit at IRCCS San Raffaele Scientific Institute, Milan, Italy, who co-chaired the session in which the study was presented, asked whether the researchers analyzed patients with optic neuritis separately from those without and whether it affected the predictive factors.
Bsteh said that OCT cannot be used for patients with bilateral optic neuritis and so they were excluded from the study, but for patients who were affected unilaterally, the contralateral eye was assessed.
This underlines why OCT contributes the most when used early on the disease course. “The longer the disease has time, the higher the likelihood that optic neuritis has developed,” he said.
Funding for the study was provided by Mindset Technologies Ltd. All authors are, or were, employees and/or shareholders of Mindset Technologies Ltd. Bsteh has relationships with Biogen, Celgene/BMS, Lilly, Merck, Novartis, Roche, Sanofi-Genzyme, and Teva.
Congress of the European Academy of Neurology (EAN) 2023: Abstract OPR-008. Presented July 1, 2023.
For more Medscape Neurology news, join us on Facebook and Twitter.
Source: Read Full Article