New research published in Blood Advances reveals that since the introduction of pneumococcal conjugate vaccines, PCV7 and PCV13, invasive pneumococcal infection (IPD) rates among children living with sickle cell disease (SCD) have declined significantly. The study explores the efficacy of existing and emerging vaccines to protect children living with SCD from life-threatening infections.
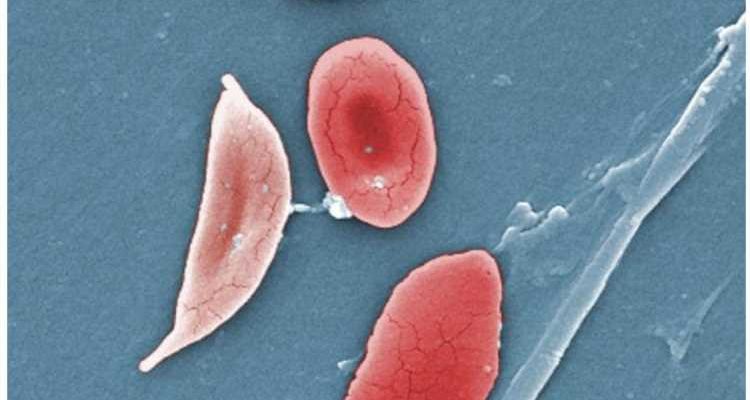
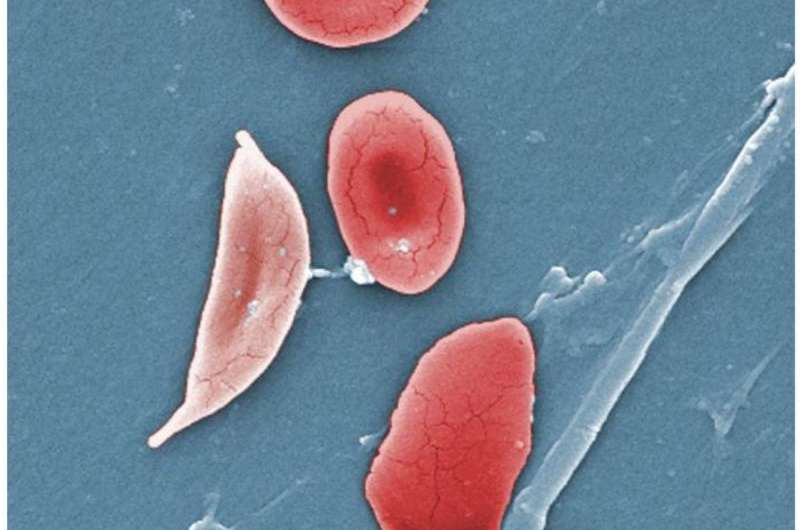
SCD is the most common inherited red blood cell disorder in the United States, affecting an estimated 100,000 people. According to the Centers for Disease Control and Prevention (CDC), SCD affects one out of every 365 Black or African American births and one out of every 16,300 Hispanic American births.
Children with SCD typically develop splenic dysfunction within their first six months to a year of life. The spleen plays a vital role in protecting the human body from infection, and children with SCD are at increased risk of developing severe, life-threatening illnesses. Those with the condition are treated with penicillin prophylaxis to reduce the risk of infection-related death.
Prior to treatment with penicillin, one in ten children per year under the age of five developed IPD, a severe infection. This accounted for 32% of all causes of death for individuals with SCD under the age of 20 in the Cooperative Study of Sickle Cell Disease. However, with antibiotic resistance on the rise over the last few decades, researchers have had to turn to new methods, such as vaccination, to protect this vulnerable population.
“In the years 2000, as pneumococci were developing antibiotic resistance, PCV7/PCV13 conjugate vaccines were introduced,” explained Thomas Adamkiewicz, M.D., MSc, a pediatric hematologist at Morehouse School of Medicine. “Since, these vaccines were developed to target bacterial serotypes not currently covered. We examined the impact of present and potential coverage of newer vaccines.”
Researchers analyzed data collected over 25 years from the Georgia Emerging Infections Program, part of the Centers for Disease Control and Prevention (CDC) Active Bacterial Core Surveillance Network, which identifies all IPD occurring in metropolitan Atlanta since 1994.
Investigators from the Georgia Emerging Infections Program, Children’s Health care of Atlanta, and Emory University collaborated in this study. They identified 104 IPD episodes in 3,707 children under 10 years old with HbSS and HbSC variants of SCD.
After 2002, 87% of children with SCD received one or more doses of the PCV7 or PCV13 vaccine in their first decade of life, according to the researcher’s data. Dr. Adamkiewicz and his team found that between 1994–1999 and 2010–2018, IPD rates declined by 87% in children from birth to four years old with HbSS, the most severe form of SCD, and by 80% in those ages five to nine.
They also identified that among children with HbSS and IPD, case fatality rates declined from 14% to 3% after 2002, and meningitis rates declined from 16% to 8%. Scientists also observed that penicillin resistance was more prevalent among this population prior to the PCV7 vaccine’s approval.
After 2000, IPD strains with serotypes emerged that were not covered by the existing PCV7 and PVC13 vaccines caused most IPDs. The older 23-valent pneumococcal polysaccharide vaccine (PPSV23) was found to be effective against pneumococcal strains with non-PCV13 serotypes, within three years after vaccination.
Investigators identified that since PCV7’s licensure, IPD rates in children with SCD ages five and older have decreased significantly. Further, since the approval and introduction of the PCV13 vaccine, no IPD infections related to the PCV13 strain have been recorded, despite some children with SCD not receiving their full recommended vaccine regimens.
These findings suggest that herd immunity, introduced by these vaccines among the general population, is helping to protect children with SCD from infection as well.
Dr. Adamkiewicz highlights that as bacterial strains with serotypes not covered by the current vaccine are predominant, children with SCD may benefit from receiving newer recently approved vaccines such as PCV15, and PCV20, which respectively cover 16% and 51% of IPD strains not covered by PCV13.
“One big question is the role of penicillin prophylaxis in children with SCD receiving new vaccines,” said Dr. Adamkiewicz. “We need far more data to make any recommendations.”
This study’s data is limited to one region of the United States, but its results might offer insights into the impact such vaccines would have on individuals with SCD in Africa—where most children with SCD reside.
While approximately two-thirds of children in the general population are reported to have received the PCV13 vaccine, mortality in children with SCD remains high, suggesting a need for wider dissemination of preventative measures, including vaccines.
In 2020, in light of this need, the ASH Consortium on Newborn Screening in Africa (CONSA)—an international network that seeks to demonstrate the benefits of newborn screening and early interventions for children with SCD in sub-Saharan Africa—was established.
While IPD remains a life-threatening risk to children with SCD, this study underscores the need for vaccines targeting broad strains of pneumococcal bacteria, and for additional research to continue advancing the prophylaxis treatments available to this population.
More information:
Blood Advances (2023).
Journal information:
Blood Advances
Source: Read Full Article