September is peripheral artery disease (PAD) awareness month. Although scientists estimate that over 200 million people worldwide suffer from the condition, it’s often neglected in the cardiovascular space in favor of more well-studied diseases, Yale scientists say.
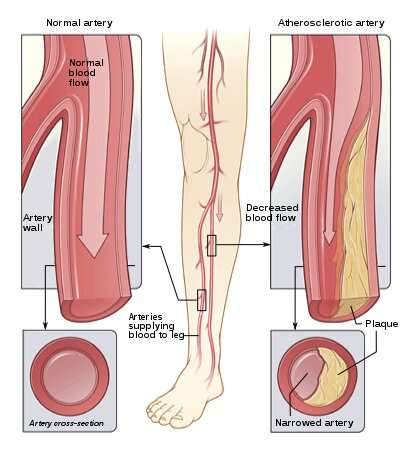
PAD is caused by blockages in the leg arteries. In the early stages of the disease, it can cause pain and other symptoms in the lower body while walking. In a more progressive stage of the disease, called critical limb ischemia, patients may experience constant pain even when not walking, which clinicians call “rest pain,” or have non-healing wounds and gangrene.
“The condition affects a large number of individuals and consumes a lot of resources from a health economic perspective, but it hasn’t gotten nearly the same amount of research, care innovations, and quality improvement initiatives compared to conditions like coronary artery disease or cerebrovascular disease,” says Kim Germaine Emiel Smolderen, Ph.D., associate professor of medicine (cardiology) and a trained psychologist. “There is a lot of unawareness that is still happening not only in the general public, but also in the medical community that needs to be addressed.”
PAD is still poorly understood, but Yale researchers are at the forefront of studying not only the disease itself, but also its close connection with mental health and how social determinants may impact health outcomes. Among Yale’s leaders are Carlos Mena-Hurtado, MD, associate professor of medicine (cardiology), who with Smolderen co-directs the recently launched Vascular Medicine OutcomeS (VAMOS) research program. Through running several parallel initiatives, the team hopes to take a more holistic approach to better understanding PAD and improving patients’ quality of life.
PAD is on the rise in younger patients
Peripheral artery disease in all of its manifestations can significantly impact a person’s quality of life. There are a variety of current interventions available depending on the severity of the disease, including managing diet, physical exercise, and medications like statins [cholesterol drugs] and anti-platelet therapies. More invasive therapies include revascularization, in which the blockage is surgically removed.
Across the world, PAD is on the rise in correlation with higher rates of obesity and diabetes. And the demographic of who gets PAD is shifting. An increasing number of younger people—those under 65 years of age—are being diagnosed with the disease.
“There are many different hypotheses for this shift,” says Mena. “One of them is the rise in comorbidities [obesity and diabetes], but the other one is the lack of adequate education both for patients and providers on the early signs and symptoms of PAD and their implications.”
PAD is closely tied to mental health
Cardiology and psychology may not seem related at first glance, but cardiovascular and mental health are intimately linked—making Mena and Smolderen a unique but important duo. PAD’s significant toll on patients’ quality of life can in turn negatively affect mood. Pain with walking often leads to reduced physical activity in PAD sufferers, and being less active also increases patients’ risk of developing depression.
Furthermore, Mena and Smolderen’s team believe there may be interrelated mechanisms between PAD and depression that have a shared pathophysiology. The inflammation seen in vascular patients has also been associated with depression. And increased platelet reactivity is also common in both conditions.
“Most likely, the relationship is multi-directional,” says Smolderen. “The increased risk of depression may be due to the experience of the disease, but also due to shared underlying mechanisms.”
Unfortunately, patients struggling with mental health still often feel a degree of stigma, which may interfere with them receiving appropriate treatment. “The stigma these patients face plays a role in the detection of their conditions, as well as the treatments they are offered,” says Mena. “So not only do we need to consider the biological association, but also the implications of how clinicians perceive their patients’ illnesses and how patients are treated.”
Yale work sheds light on PAD and mental health
To learn more about the link between PAD and mental health, Mena and Smolderen are leading multiple initiatives. Through utilizing national quality registries, their team is looking at trends related to how psychiatric co-morbidities may affect risk of procedural complications. And mental health disorders in patients, they are finding, may make patients more likely to suffer poorer outcomes. Critical limb ischemia patients with depression or anxiety, for example, are at greater risk of amputation.
They also are leading a multi-center study called SCOPE-CLI, which spans across 10 centers in the United States and one in Australia. The study is following patients newly diagnosed with critical limb ischemia to better understand its impact on mood and quality of life.
Other ongoing research focuses on pain management strategies in those suffering from advanced PAD. Preliminary evidence suggests that there may be increased opioid use in this group. This may place the patients at risk for worsening disease progression, complications, and depression. The team also hopes to better understand the relationship between advanced PAD and addiction disorders.
Smolderen and Mena hope to use their insights to develop intervention programs that they can pilot in the clinic and around which they can develop develop integrated behavioral health interventions.
Social determinants can affect PAD outcomes
Studies also show that higher concentrations of PAD occur in areas that also suffer from high stress and deprivation. Access to high quality food options and places to exercise also play an important role. “We believe that exposure to more distressed circumstances and more access-to-care barriers increases your risk of getting the disease and also getting detected later for the disease,” says Smolderen.
A recent study by Smolderen and Mena’s team also found that those of Hispanic ethnicity may be at increased risk of worsened outcomes. Their research showed that Hispanics are more likely to receive care for PAD at later stages of the disease compared to white patients, and that they predominantly receive their care through the emergency department. Due to this disparity, they are also at a higher risk of amputation due to the disease.
“The number of Hispanics in the United States is rising, and as a Hispanic myself, trying to understand the intricacies of our culture is incredibly important,” says Mena. “The differences in the way they are treated is quite significant and highlights they need more help, effort, and resources.”
Investigating PAD is a team effort
Smolderen and Mena are grateful for the many collaborators at Yale who make their efforts possible. “Even though Kim and I are the leaders of the program, and I certainly couldn’t do this without her, I think that credit must go to the many other people involved, from the analysts to all the different trainees, medical students, and residents,” says Mena. “Both the university and the hospital side play a major role in supporting our efforts and investigations.”
Source: Read Full Article
