Moving in a very different direction from past coronary stent designs, a new device that is being characterized as bioadaptable, as opposed to bioabsorbable, was noninferior to a widely used drug-eluting stent, and associated with several unique vessel functional improvements at 12 months in a randomized controlled trial.
“The device restored vessel motion, which we think is the reason that we saw plaque stabilization and regression,” reported Shigero Saito, MD, director of the catheterization laboratory at Shonan Kamakura (Japan) General Hospital.
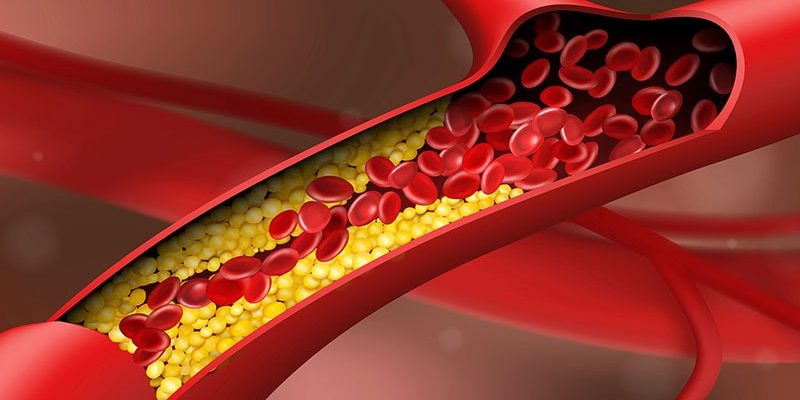
The principal features of the bioadaptable design are cobalt-chromium metal helical strands to provide indefinite scaffolding support coupled with a biodegradable sirolimus-containing poly(D,L-lacti-co-glycolic acid) (PLGA) topcoat and a biodegradable poly-L-lactic acid (PLLA) bottom coat to “uncage” the vessel once these materials are resorbed, said Dr. Saito.
Twelve-month data from the randomized BIOADAPTER trial, presented as a late breaker the annual meeting of the European Association of Percutaneous Cardiovascular Interventions, provide the first evidence that this uncaging of the vessel is an advantage.
Compared head-to-head in a contemporary drug-eluting stent (DES) in a randomized trial, the bioadaptable stent, as predicted in prior studies, “improved hemodynamics and supported plaque stabilization and positive remodeling,” said Dr. Saito.
In BIOADAPTER, 445 patients in Japan, Germany, Belgium, and New Zealand were randomized to the novel stent, called DynamX, or to the Resolute Onyx. The trial has a planned follow-up of 5 years.
While the primary endpoint at 12 months was noninferiority for target lesion failure (TLF), it was a series of secondary imaging endpoints that suggest an important impact of uncaging the vessel. This includes better vessel function potentially relevant to resistance to restenosis.
As a result of numerically lower TLF in the DynamX group (1.8% vs. 2.8%), the new device easily demonstrated noninferiority at a high level of significance (P < .001). A numerical advantage for most events, including cardiovascular death (0% vs. 0.9%) and target-vessel myocardial infarction (1.4% vs. 1.9%), favored the novel device, but event rates were low in both arms and none of these differences were statistically significant.
However, the secondary imaging analyses at 12 months suggested major differences between the two devices from “uncaging” the vessel.
These differences included a highly significant improvement at 12 months in vessel pulsatility (P < .001) within the DynamX stent relative to the Onyx stent in all measured segments (proximal, mid, and distal).
In addition, compliance remained suppressed relative to both the proximal (P < .001) and distal (P < .001) vessels of patients fitted with Onyx device. Conversely, there was no significant relative difference in this measure among those fitted with the DynamX device.
At 12 months, the plaque volume change behind the stent of noncalcified lesions increased 9% in the Onyx group but was reduced 4% in the DynamX group (P = .028).
While there was a 13% gain overall in percent diameter stenosis within the stent of patients receiving the DynamX device, it was consistently lower than that observed in the Onyx group. This difference was only a trend overall (12.7% vs. 17.3%; P = .051), but the advantage reached significance, favoring DynamX, for the left anterior descending (LAD) artery (12.1% vs. 19.0%; P = .006), small vessels (13.0% vs. 18.3%; P = .045), and long lesions (13.0% vs. 22.9%; P = .008).
The same relative advantage for DynamX was seen on late lumen loss at 6 months. In this case, the overall advantage of DynamX (0.09 vs. 0.25; P = .038) did reach significance, and there was an advantage for the LAD (–0.02 vs. 0.24; P = .007) and long lesions (–0.06 vs. 0.38; P = .016). The difference did not reach significance for small vessels (0.08 vs. 0.26; P = .121).
All of these advantages on the secondary endpoints can be directly attributed to the effect of uncaging the vessel, according to Dr. Saito, who said this new design “addresses the shortcomings” of both previous drug-eluting and biodegradable stents.
Pointing out that the nonplateauing of late events has persisted regardless of stent design after “more than 20 years of innovation in design and materials,” Dr. Saito said all current stents have weaknesses. While biodegradable stents have not improved long-term outcomes relative to DES “as a result of loss of long-term vessel dynamic support,” DES are flawed due to “permanent caging of the vessel and loss of vessel motion and function.”
This novel hybrid design, employing both metal and biodegradable components, “is a completely different concept,” said Ron Waksman, MD, associate director, division of cardiology, Medstar Hospital Center, Washington. He was particularly impressed by the improvements in pulsatility and compliance in target vessels along with the favorable effects on plaque volume.
“The reduction in plaque volume is something we have not seen before. Usually we see the opposite,” Dr. Waksman said.
“Clearly, the Bioadapter device is not a me-too stent,” he said. He was not surprised that there was no difference in hard outcomes given both the small sample size and the fact that the advantages of uncaging the vessel are likely to accrue over time.
“We need to look at what happens after 1 year. We still have not seen the potential of this device,” he said, adding he was “impressed” by the features of this novel concept. However, he suggested the advantages remain theoretical from the clinical standpoint, advising Dr. Saito that “you still need to demonstrate the clinical benefits.”
Dr. Saito reports a financial relationship with Elixir Medical, which funded the BIOADAPTER trial. Dr. Waksman reports financial relationships with 19 pharmaceutical companies including those that manufacture cardiovascular stents.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article