TOPLINE:
Genetic testing may help identify patients with Barrett esophagus who are at highest risk for progression to esophageal adenocarcinoma.
METHODOLOGY:
-
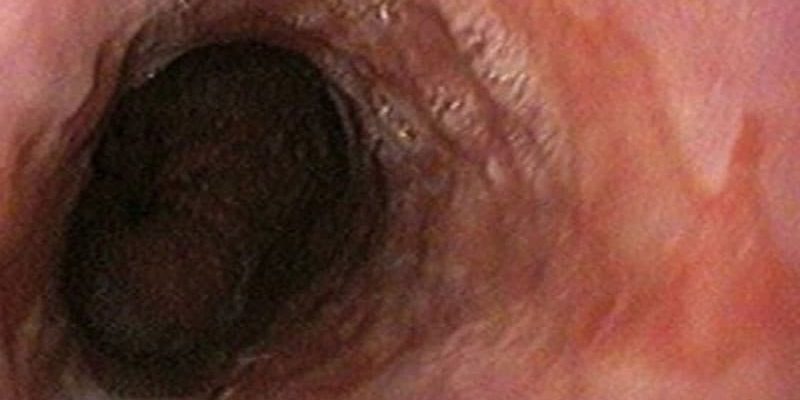
About 7% of middle-aged adults have Barrett esophagus, but in only a small percentage of patients (0.12% to 0.5%) does the condition progress to esophageal adenocarcinoma each year.
-
In the current study, 640 patients with Barrett esophagus and high-grade dysplasia or esophageal adenocarcinoma were tested for the presence and frequency of cancer-predisposing genes.
-
Participants underwent either whole-genome sequencing or whole-exome sequencing.
-
The investigators compared the frequency of pathogenic germline mutations in monoallelic cancer-predisposing genes between patients who had experienced progression and those who had not.
TAKEAWAY:
-
Pathogenic germline mutations were identified in 9% of patients (59 of 640) with Barrett esophagus who had high-grade dysplasia or esophageal adenocarcinoma and in only 2.7% of those who did not experience progression.
-
ATM and CHEK2 were the most frequently mutated genes. Mutations in these genes occurred, respectively, in 1.6% and 1.25% of participants who experienced progression to esophageal adenocarcinoma. Five participants (0.8%) had germline mutations in TP53, and two (0.3%) had distinct, splice-donor mutations in CDH1 at intron 10.
-
Progression to esophageal adenocarcinoma in patients with mutations was seen across the age spectrum, suggesting that additional triggers, such as having Barrett esophagus and experiencing environmental exposures, may be necessary for carcinogenesis.
IN PRACTICE:
The findings suggest that certain “mutations facilitate the progression of Barrett’s esophagus to adenocarcinoma,” the authors said. For patients who experience progression toward esophageal adenocarcinoma from Barrett esophagus, “performing genetic testing is probably warranted.”
SOURCE:
The study was published online July 26 in Gastroenterology.
LIMITATIONS:
It was a retrospective database study.
DISCLOSURES:
The research was supported by the Elsa U. Pardee Foundation, the American College of Gastroenterology, and the National Institute of Diabetes and Digestive and Kidney Diseases. The authors have disclosed no relevant financial relationships.
Neil Osterweil, an award-winning medical journalist, is a long-standing and frequent contributor to Medscape.
For more from Medscape Oncology, join us on Twitter and Facebook.
Source: Read Full Article