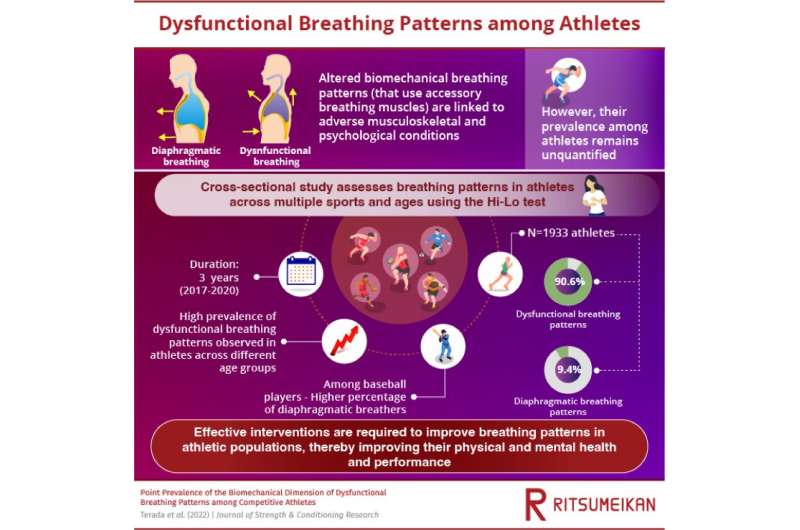
Dysfunctional breathing patterns are associated with a high risk of musculoskeletal conditions, resulting in poor physical performance. Now, a study by researchers in Japan has found that among athletes across age groups, there is a high prevalence of dysfunctional breathing patterns. Effective intervention strategies are required to restore normal breathing patterns and prevent injuries among athletes to ensure their superior performance and health.
Breathing patterns are an important indicator of an individual’s health. A healthy individual breathes naturally using primary respiratory muscles (e.g., diaphragm muscle) that produce a rhythmic observable movement of the upper rib cage, lower rib cage, and abdomen. This is known as the diaphragmatic breathing pattern, which has been associated with improvements in posture, core stability, and functional performance, as well as reductions in musculoskeletal injury, pain, and stress.
In contrast, individuals with altered or dysfunctional biomechanical breathing patterns are unable to contract their diaphragm to a desired extent and begin relying on accessory respiratory muscles to breathe. They display superior rib cage movement and shoulder elevation, reduced abdominal movements, and lateral rib cage expansion.
Previous research suggests a strong association between altered biomechanical breathing patterns and the development of musculoskeletal conditions, such as lower back pain, neck pain, chronic ankle instability, and temporomandibular joint disorders.
Superior physical performance and prevention of musculoskeletal injuries are crucial for athletes to deliver their best performance at competitive sports. Evidence from previous studies suggests that athletes with diaphragmatic breathing patterns display improved physical and psychological performance. But since athletes with altered breathing patterns might be at an enhanced risk of developing musculoskeletal injuries, identifying the prevalence of altered breathing patterns is of utmost importance to prevent them from developing injuries.
Now, a team of researchers led by Dr. Terada from Ritsumeikan University in Japan has conducted a novel study, published in the Journal of Strength and Conditioning Research , to examine the prevalence of dysfunctional and diaphragmatic breathing patterns in an athletic population, and determine the biomechanical dimensions of these breathing patterns.
The team tested 1,933 competitive athletes from schools in Japan, across multiple sports and ages during 2017 and 2020, using a Hi-Lo test—a test that identifies an individual’s breathing pattern. Scores for the Hi-Lo test were determined based on the presence or absence of abdominal excursion, anterior-posterior chest expansion, superior rib cage migration and shoulder elevation. The team further classified these participants into thoracic-dominant and abdomen-only breathers based on the presence of abdominal excursion.
Findings indicate that an alarmingly high proportion (91%) of the athletes displayed dysfunctional breathing patterns, while only 9.4% of them displayed diaphragmatic breathing patterns. In fact, among athletes who played baseball, there was a greater percentage of diaphragmatic breathers than that among those who played tennis, basketball, badminton, and volleyball. This indicates that athletes’ breathing patterns vary depending on the type of sport they are involved in, since each sport has different energy demands and constraints.
Moreover, the team observed that the highest proportion of dysfunctional breathers were middle school student athletes, followed by elementary school student athletes, and high school student athletes. The proportion of collegiate athletes with dysfunctional breathing patterns was slightly lower in comparison.
Further, among the population identified as dysfunctional breathers, 61% of the athletes were found to be thoracic-dominant breathers, as compared to the 39% abdomen-only breathers.
These findings suggest an overall high prevalence of dysfunctional breathing patterns in the athletic population across age groups, which requires immediate addressing as an important sports-medicine issue.
When asked about the implications of these findings, Dr. Terada said “Clinicians need to consider screening breathing patterns and implementing corrective approaches targeted at specific components of dysfunctional breathing patterns. They should also consider evaluating sport-specific adaptations of breathing and implementing sport-specific breathing training protocols.”
Source: Read Full Article