The human immune system doesn’t just protect our health, it reflects it. Each encounter with a potential disease-causing agent causes the body to produce specific immune agents—proteins known as antibodies and T-cell receptors—tailor-made to recognize and destroy the invader. Tasked with preventing re-infection, antibodies and T-cell receptors (TCR) from your previous encounters circulate throughout the body indefinitely, like a record of your personal medical history that you carry inside of you.
Clinical pathologist Ramy Arnaout, MD, DPhil, Associate Director of the Clinical Microbiology Laboratories at Beth Israel Deaconess Medical Center, wants to mine those personal medical records for information. In a recent perspective published in Frontiers in Immunology, Arnaout and colleagues in the Adaptive Immune Receptor Repertoire Community (AIRR-C) outline how the immunome—all of the genes collectively expressed by an individual’s immune cells—holds the potential to provide researchers and physicians with unprecedented insight into an individual’s health. Collecting that information from large numbers of patients could one day facilitate diagnostics via a near-universal blood test and pave the way to targeted therapies for a wide variety of conditions.
We asked Dr. Arnaout to tell us more about this new frontier of personalized medicine.
What exactly is the immunome and what can researchers and physicians learn from it?
The immunome is the complete set of immune cells—antibodies and T cell receptors (TCR)—that every person makes in response to infections, vaccinations, transplants and transfusions, autoimmune diseases, aging and cancers.
Right now, you have in your body something like a hundred billion to a trillion T and B cells, minding their own business, circulating through your blood, leaving to check out what’s going on in all your organs, and then completing the loop and coming back around.
A number of us in the field have been thinking for some time that if we could just figure out which antibodies and T-cell receptors match to which disease or condition, then we would have a universal diagnostic. That is, we would be able to look at a person’s antibodies and T-cell receptors, and just by seeing what’s there, we’d be able to say, “Oh, these antibodies are against melanoma, that means you probably had it, but your immune system took care of it,” or, “You probably had the flu.”
One blood test, one jab—everything else is computer science on the other end. But first we need to crack that code.
What could researchers and physicians do with this information?
If I looked at your immunome and your friend’s immunome, you might assume that you’d have nothing in common. But, despite the underlying differences among us all, the antibodies and TCR we produce are similar enough even if they are not identical that scientists can look at them bioinformatically and recognize patterns.
We know now from data that despite extraordinary, unfathomable potential of diversity—there are more different possible sequences than stars in the observable universe, certainly more than grams of mass in the sun—you and I are not genetically that different. We live in the same world, we’re sneezed on by the same people on the subway—it is incredible that our actual diversity genetically is so unbelievably constrained that we have been able to and regularly do find patterns that we might have thought couldn’t exist ten years ago.
So, by getting samples from people who have known conditions—such as COVID-19, dengue, ebola and other infectious diseases—and comparing them to control samples, scientists can computationally pull out patterns.
But the missing ingredient here is you. In this paper my colleagues and I just published in Frontiers in Immunology, we’re trying to announce to the scientific community and beyond that we can find these patterns and put them to good use. But we need clinicians to be aware of this and connect with us.
For example, say an endocrinologist has a patient with a benign thyroid growth. In principle, we could take a sample of that patient’s blood, find a sequence, and then use that sequence as an early diagnostic tool for future patients.
What technology is required to decode the immunome?
Step one was sequencing. Sequencing was the technology that made this kind of thinking possible. We now have the ability to sequence these antibody and TCR genes so that we can actually see what’s in there.
Now that sequencing is more of a commodity, the frontier has moved to ‘how can we find the patterns?’ That’s the mathematical and computational side of things, processing the sequencing data with artificial intelligence or machine learning algorithms.
But I don’t want to overlook this third plank, even though it’s not as splashy as sequencing and artificial intelligence: As I said before, the missing ingredient is you. We are past due for a nationwide, learning healthcare system.
Can we make sure that if a patient comes into a hospital in Massachusetts or Maine or Missouri, we can eventually get access to that blood sample that’s about to be thrown out long after the patient has gone home, and sequence the millions of antibody and TCR genes it contains? And in addition to access to these discarded specimens across medical systems, we need them correlated to the information in electronic health records (EHR).
With the immunome, we have the chance again to use sequencing to learn about an individual’s health, add that information to a database, correlate it to that person’s health record, times millions of individuals—we can untangle this code in relatively short order.
What is the good faith critique of this line of thought?
There is a point of view that if you want to diagnose an infection, for example, why look for the response? Just look for the infectious agent itself, right? Or if you want to see how person responds to cancer treatment, why look at the adaptive response of the immune as an indicator—why not test cancer cells against drug? These are reasonable questions.
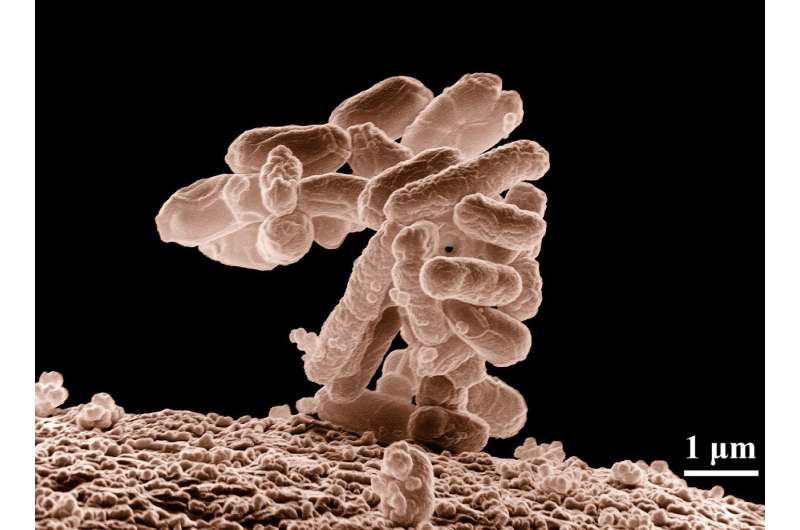
The answer is, the body takes a lot of these insults very seriously. Even if you have a rip-roaring, potentially life-threatening infection, the number of viable bacteria per milliliter of blood is vanishingly small—around one viable bacterium per 5-10 milliliters of blood. Maybe there’s a lot of bacteria somewhere in your body. But more typically, your body just takes infection with bacteria very seriously, so just a few bacteria are enough to set off a cascade of events that can kill you. Finding the actual bacteria, and distinguishing it from random bacterial DNA flotsam in the blood, is harder than it is to look at a person and say, “this person’s white blood cell count is through the roof.”
In other words, the immune response is not a proportional response, it’s often a massively disproportionately response in many cases. It acts as a signal amplifier from a diagnostic perspective, and that’s an advantage. If we can get enough samples to recognize a pattern, and if we can get enough samples, the track-record so far suggests we can determine what that signal is.
Why did you and your colleagues publish this Frontiers in Immunology paper now?
The Adaptive Immune Receptor Repertoire Community (AIRR-C) is a dedicated community that we wrote this paper with and on behalf of. We have the knowledge and expertise to lay the groundwork for the diagnostic potential of the immunome, but we can go so much faster with the help of others. That’s why we are putting out a call to clinicians, researchers and others to join efforts with AIRR-C.
My hope is the next generation of doctors in medical school, when they hear about this they think, “I want to work on that.”
Source: Read Full Article
