A new phase I clinical study shows, for the first time, how treatment with a type of stem cell called mesenchymal stromal cells is able to regulate important factors driving inflammation in patients with chronic obstructive pulmonary disease (COPD) for a period for time. The study, whose results were released in Stem Cells Translational Medicine, provides insights that may aid in developing a new cellular therapy for treating COPD which is among the top five causes of morbidity and mortality worldwide—and other chronic airway diseases.
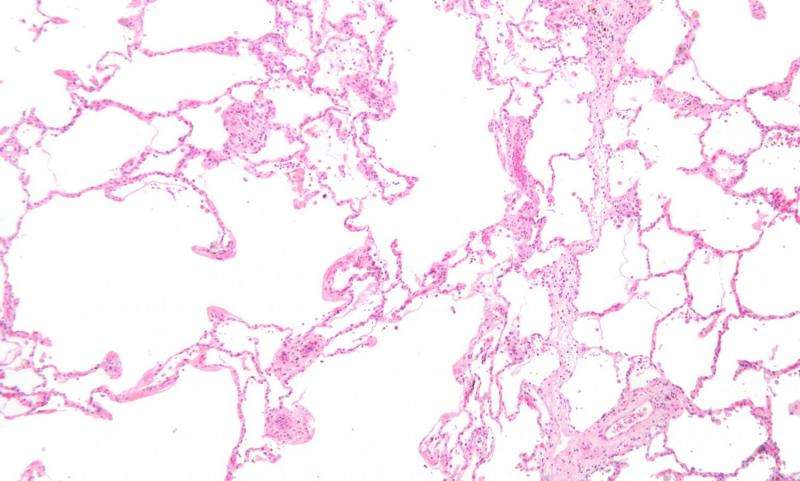
COPD is a chronic inflammatory lung condition that obstructs airflow from the lungs. It is generally caused by long-term exposure to irritating gasses or particulate matter, most often cigarette smoke. Symptoms include difficulty breathing, chronic cough, lack of energy, wheezing and frequent respiratory infections. People with COPD are also at an increased risk of developing other serious diseases such as heart disease and lung cancer.
Treatments are available to help a patient cope with COPD, but there is no cure and the disease progressively worsens over time. With limited therapeutic options, researchers have been exploring various cell-based therapies as a way to regenerate COPD-damaged lung tissue. Mesenchymal stromal cells (MSCs) in particular have attracted attention. These multipotent adult stem cells are present in umbilical cord, bone marrow, fat, dental and other body tissues. Their ability to secrete biologically active molecules that exert beneficial effects on injured tissues and relieve chronic inflammation has made them a promising candidate in regenerative medicine.
Preclinical studies in which rodents with COPD were treated with MSCs showed they alleviated inflammation and reduced emphysema; however, these findings have translated poorly in human studies. Why is unclear—and is something that is underscored by a lack of mechanistic studies in humans to determine how MSCs impact COPD inflammation.
The team of researchers behind this latest study had previously shown that MSC infusions are well tolerated in patients with COPD and reduce biomarkers associated with systemic inflammation and oxidative stress.
“This time we wanted to delineate the underlying mechanisms further by characterizing the transcriptional networks in these patients, which are the proteins that turn genes on and off to ensure that they are expressed in the right cell at the right time and in the right amount, and to explore the role of MSCs in regulating these pathways,” said study leader Yuben P. Moodley, M.D., Ph.D., head of the Cell Biology Unit at the Institute for Respiratory Health, a consultant respiratory physician at Fiona Stanley Hospital and associate professor of respiratory medicine at the University of Western Australia. He teamed up with colleagues from these institutions as well as from Royal Perth Hospital to conduct the clinical study.
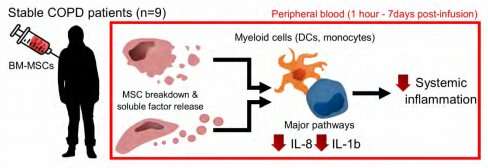
Nine patients with stabilized COPD—all of whom had participated in the earlier study—were treated with an infusion of MSCs extracted from the bone marrow of donors. Gene expression profiles from peripheral blood mononuclear cells (PBMCs) were analyzed during the first week after infusion.
The results indicated that the MSCs did, indeed, reduce important disease-causing pathways behind chronic airways disease and that MSC-derived soluble factors may be responsible for these changes. “Our investigation also outlined several potential paracrine mechanisms that may be exerting these effects, demonstrating the therapeutic potential of media from which MSC are cultured (MSC-CM),” Dr. Moodley said.
However, the results also revealed that seven days after treatment, the MSCs beneficial effects began to wane.
“This is in line with a recent study in patients with septic shock receiving MSC infusions, where inflammatory levels were most prominently reduced around 12 to 24 hours after infusion, then reverted to baseline levels in the subsequent days. These effects are likely a consequence of the rapid breakdown of MSCs following intravenous infusion.
“This suggests that frequent, perhaps weekly doses, may be important to achieve clinical benefit in COPD patients,” Dr. Moodley said. “The insights gained from this study warrant further investigation of MSCs and/or their secreted factors as a novel therapeutic intervention in chronic airways diseases,” he added.
Source: Read Full Article
