Coronaviruses are a global public health risk, with three highly infectious species, including SARS-CoV-2, emerging in the last 20 years. New research by the University of Bristol has shown how an HIV drug could stop many coronavirus diseases, including the SARS-CoV-2 variants, when given to infected cells at the right concentration. The findings could strengthen the arsenal of antiviral drugs available to combat current and future coronavirus outbreaks.
Currently, there are limited antiviral therapies available against SARS-CoV-2—the virus that causes COVID-19, and these drugs are not always effective, highlighting the need for more treatments. Also, the virus can mutate, and its variants can become partially or completely resistant to some of the available treatments, such as monoclonal antibodies.
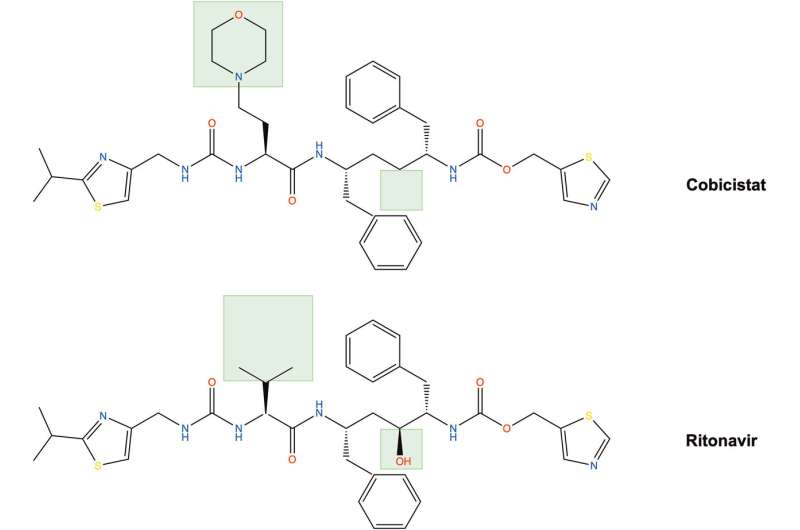
The research team has previously shown that a booster drug (cobicistat), which is normally used to reinforce the effect of anti-HIV drugs, could have antiviral properties against a SARS-CoV-2 variant circulating in Europe in early 2020.
In this study, published in Antiviral Research today (5 December) the researchers studied whether the anti-SARS-CoV-2 properties of cobicistat were maintained against the key variants of concern (VOCs) of SARS-CoV-2 and other coronaviruses, including Middle East respiratory syndrome coronavirus (MERS-CoV).
MERS-CoV circulates in the Middle East, Africa and South Asia and has a death rate of more than 30% with no vaccine or specific treatments being currently available. The team also compared the effects of cobicistat to those of ritonavir, which is a structurally similar molecule and also one of the components of Paxlovid, which is the current gold standard for antiviral treatment of SARS-CoV-2.
The research, using automated image analysis for a screening and parallel comparison of the anti-coronavirus effects of cobicistat and ritonavir, found cobicistat and ritonavir both act against all eight VOCs of SARS-CoV-2 that were tested as well as against other human coronaviruses, including MERS-CoV.
The findings indicate that cobicistat is more powerful than ritonavir. Both drugs displayed anti-coronavirus activity in vitro at dosages that are well tolerated, but higher than those currently used for booster activity of anti-HIV drugs and in Paxlovid. When used at these higher dosages cobicistat and ritonavir both inhibited coronavirus replication on their own and when combined with other drugs.
Dr. Iart Luca Shytaj, lecturer in the school of cellular and molecular medicine and one of the paper’s corresponding authors, said, “Our results indicate that cobicistat, at dosages above its typical clinical use as a booster, could become an effective antiviral drug both on its own and in combination with other antivirals and lead to more potent treatments than current available options.
“If our findings are confirmed in animal and clinical studies, our results could strengthen the arsenal of antiviral drugs in the fight against current and future outbreaks of coronaviruses and reduce their impact on public health globally.”
Next steps for the research include animal and clinical testing of high-dose cobicistat in combination with the other component of Paxlovid, nirmatrelvir, as first treatment against MERS-CoV infection.
More information:
Lara Gallucci et al, Broad-spectrum antiviral activity of two structurally analogous CYP3A inhibitors against pathogenic human coronaviruses in vitro, Antiviral Research (2023). DOI: 10.1016/j.antiviral.2023.105766
Journal information:
Antiviral Research
Source: Read Full Article
