Before SARS-CoV-2, the virus that causes COVID-19, spread across the world in 2020, tuberculosis was responsible for more deaths globally than any other infectious disease. But thanks to targeted public health efforts in the U.S. and globally, tuberculosis cases had been steadily falling for decades.
I am an infectious disease clinician and public health practitioner who has been caring for underserved communities in the U.S. for more than two decades.
During the pandemic, it at first appeared that, as with many other common illnesses like the flu, COVID-19 prevention efforts reduced tuberculosis cases, too. But tuberculosis numbers have quickly climbed back up to pre-pandemic levels, marking the first time in decades that cases and deaths have risen globally.
The pandemic not only interrupted important health interventions for tuberculosis, it also caused a decrease in social and economic opportunities for marginalized people around the globe. Together, these effects appear to have put a serious dent in the fight against tuberculosis.
Tuberculosis before and during COVID-19
Tuberculosis is a contagious bacterial infection of the lungs that is normally spread through the air. Most tuberculosis infections are asymptomatic and not contagious.
About 5% to 10% of infected individuals develop active tuberculosis, which is characterized by cough, fever, decreased appetite and weight loss. If left untreated, tuberculosis is a very contagious and dangerous disease that can result in death.
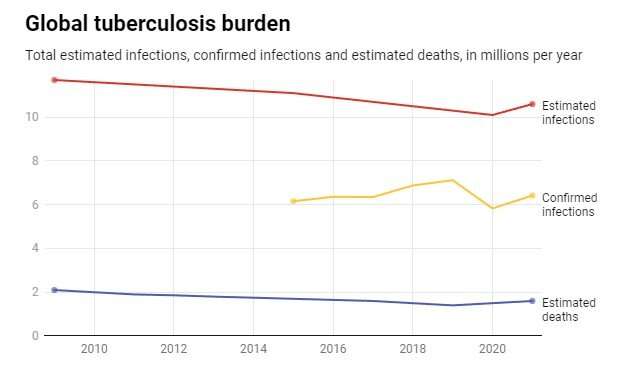
Total estimated tuberculosis infections globally have been falling for years. The lowest number, 10.1 million cases, occurred in 2020, according to the World Health Organization. 2021 saw a significant increase in infections, to 10.5 million, the first rise in more than a decade. Global tuberculosis deaths followed a similar pattern, reaching a low point of an estimated 1.4 millions deaths in 2019, then rising to 1.5 million in 2020 and 1.6 million in 2021.
The number of confirmed cases of tuberculosis—infections detected through direct testing—tells a different part of the story. As testing efforts have improved, confirmed cases have been rising globally to a peak in 2019. As the coronavirus disrupted lives in 2020, confirmed cases of tuberculosis fell significantly before quickly rising again in 2021.
A similar pattern played out in the U.S. There was a sharp drop in confirmed cases in 2020—mostly driven by lack of testing—followed by a sharp rise back to pre-pandemic levels.
Tuberculosis is a social disease
Tuberculosis is a preventable disease, thanks to effective vaccines, testing and treatments. But millions of people around the world still suffer from this disease, not because of a lack of medical knowledge, but because of persistent social inequities.
Unequal access to economic opportunities, limited health care, poor sanitation, crowded living conditions, malnutrition and illnesses such as diabetes or HIV are all associated with increased risk of tuberculosis.
In the U.S. in 2021, racial and ethnic minority groups accounted for more than 85% of tuberculosis cases, with 71% of cases occurring in persons born outside the U.S.
Increased inequality causing more tuberculosis
Even as the world witnessed a rapid decline in confirmed cases in 2020, experts were worried that interruption of prevention and treatment efforts might result in a rise in tuberculosis.
These fears were warranted. Many health experts, along with the U.S. Centers for Disease Control and Prevention, have confirmed the pandemic disrupted access to tuberculosis testing and diagnosis. It is likely that many cases were missed because of the interruption of tuberculosis control activities, since funding, resources and staff were reassigned to assist in COVID-19 control efforts. Additionally, during health encounters, similarities in symptoms between COVID-19 and tuberculosis may have led to missed diagnoses.
The drop in confirmed cases seems to be, in large part, driven by a lack of testing. The rapid increase since the pandemic, and especially the rise in deaths, confirms that progress made in tuberculosis control over the past 20 years has stalled, slowed or reversed. These two troubling trends are also almost certainly connected to the increase in inequality brought about by the pandemic.
The existence of multigenerational households, overcrowding in low-income neighborhoods, lack of paid sick leave, inability to shield from the pandemic, use of public transportation and lack of health insurance all converged to heighten the risk of both COVID-19 and tuberculosis among the most vulnerable people.
Of course, the pandemic is not the only factor that has increased human hardship—and therefore, tuberculosis—in recent years. For example, Ukraine now has one of the world’s highest tuberculosis disease burdens as a result of Russia’s invasion and the resulting harm to Ukraine’s medical, social and economic systems. Ongoing conflicts in other parts of the world, energy shortages and the effects of climate change and associated impacts on food security are expected to worsen the broader social and political determinants of tuberculosis.
There are many neglected diseases of poverty, and tuberculosis is a great example of how social forces produce human disease. With an estimated one-third of the world’s population at risk for tuberculosis today, fostering social justice interventions to reduce health inequities is a critically important step to relieving the global medical burden of this relentless disease.
Provided by
The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: Read Full Article
