Over the past 21 years of opioid overdose deaths—from prescription drugs to heroin to synthetic and semisynthetic opioids such as fentanyl—geography has played a role in where opioid-involved overdose deaths have occurred, reports a new Northwestern Medicine study.
But the coming wave will not discriminate between rural and urban areas, the study findings suggest. Every type of county—from the most rural to the most urban—is predicted to see dramatic increases in deaths from opioid-involved overdoses. The reason opioid overdoses have reached historical highs comes from combining synthetic opioids with stimulants such as cocaine and methamphetamines, a lethal cocktail that is hard to reverse during an overdose, the study authors said.
“I’m sounding the alarm because, for the first time, there is a convergence and escalation of acceleration rates for every type of rural and urban county,” said corresponding author Lori Post, director of the Buehler Center for Health Policy and Economics at Northwestern University Feinberg School of Medicine. “Not only is the death rate from an opioid at an all-time high, but the acceleration of that death rate signals explosive exponential growth that is even larger than an already historic high.”
The study will be published July 28 in JAMA Network Open.
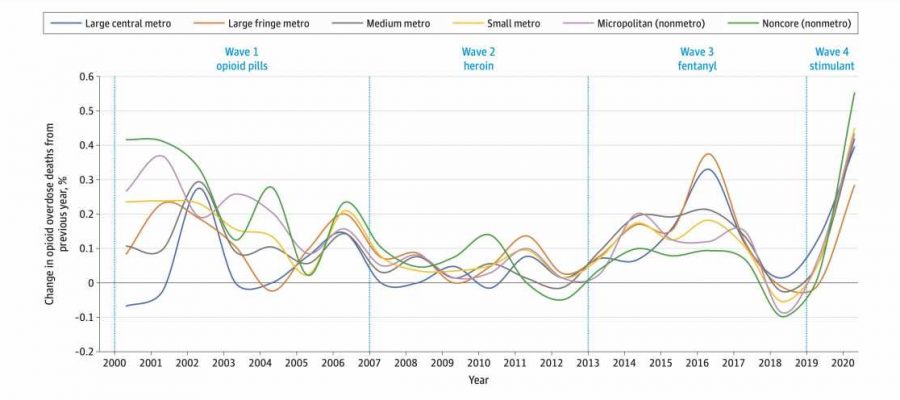
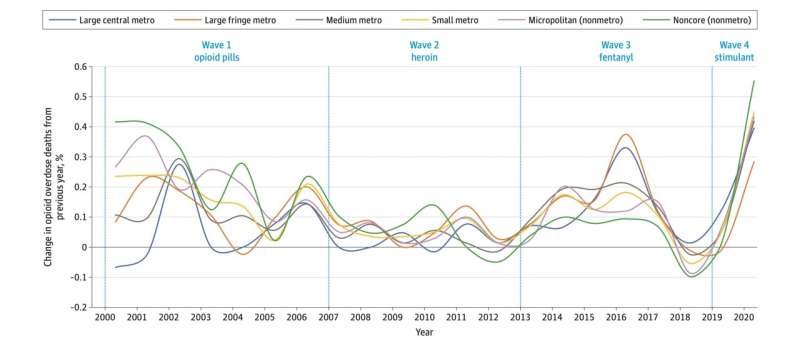
The study examined geographic trends in opioid-involved overdose deaths between 1999 and 2020 to determine if geography played a role in the three waves and the theorized fourth wave of America’s opioid crisis. The authors used data recorded in the Centers for Disease Control and Prevention’s WONDER database for 3,147 counties and county equivalents categorized on a six-point urbanicity scale (most urban to most rural).
First study to look at acceleration rates systematically by geography
While some researchers have looked at an acceleration rate from one year to the next, the study authors said, to their knowledge, no one has examined acceleration rates of opioid-involved overdose death rates systematically by geography for every year.
Post used methods she developed to assess where COVID-19 outbreaks were brewing and applied them to opioid misuse.
Near the end of the available data from 2020, overdose deaths in rural areas were escalating faster than in urban areas, according to the study. A visualization of the data illustrates that between 2019 and 2020, rates of opioid-involved overdose deaths converged while escalating for the first time across six types of rural and urban counties, Post said.
“We have the highest escalation rate for the first time in America, and this fourth wave will be worse than it’s ever been before,” Post said. “It’s going to mean mass death.”
A lethal combination
The study authors examined toxicology reports and found people are using fentanyl (a synthetic opioid that is 50 to 100 times more potent than morphine) and carfentanil (a synthetic opioid approximately 100 times more potent than fentanyl) combined with methamphetamines and cocaine. The result is a powerful and lethal cocktail that can even evade help from overdose-reversing drugs like naloxone.
“The stronger the drugs, the harder it is to revive a person,” said study co-author Alexander Lundberg, assistant professor of emergency medicine at Feinberg. “The polysubstance use complicates an already dire situation.”
“It appears that those who have died from opioid overdoses had been playing pharmacist and trying to manage their own dosing,” Post said. “This is a bigger problem because you have people misusing cocaine and methamphetamines along with an opioid, so you have to treat two things at once, and the fentanyl is horribly volatile.”
What can be done?
“Nobody wants to be a drug addict,” Post said. “It doesn’t matter if you’re taking Percocet because you broke your back while mining or if you’re a high schooler who died because they got into grandma’s medicine cabinet. We need to look at opioid-addiction and overdose prevention immediately.”
That might be in the form of methadone or buprenorphine centers, which offer medication-assisted anti-addiction treatments for heroin or synthetic and semisynthetic opioid overdoses, Post said, although they are typically only opened in urban areas. Rural areas have no medication-assisted treatment options, she said, adding that what works in large cities is likely not as useful for rural areas.
“The only path forward is to increase awareness to prevent opioid use disorders and to provide medication-assisted treatment that is culturally appropriate and non-stigmatizing in rural communities,” Post said.
Source: Read Full Article