Formation of new blood vessels can be divided into two processes – vasculogenesis and angiogenesis. Vasculogenesis represents the formation of new blood vessels from hemangioblasts during embryonic development, while angiogenesis is the formation of new capillary branches from established blood vessels.
Skip to:
- What is Vascular Endothelial Growth Factor?
- How is VEGF production triggered?
- How does VEGF stimulate the growth of new blood vessels?
- What are the normal roles of VEGF?
- What roles does VEGF play in cancer?
 Vascular Endothelial Growth Factor?” />
Vascular Endothelial Growth Factor?” />
What is Vascular Endothelial Growth Factor?
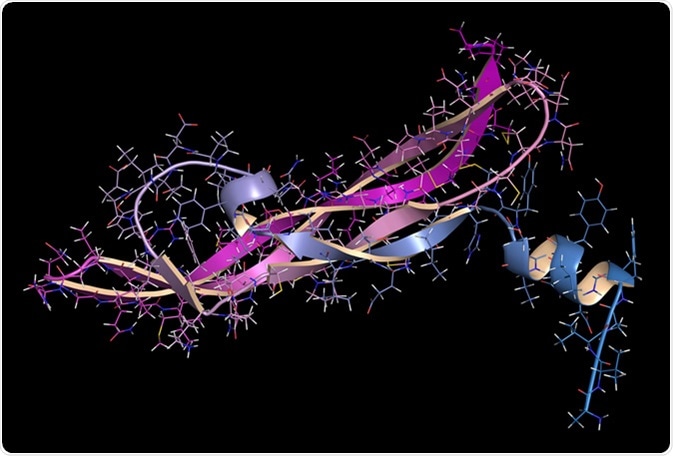
Vascular Endothelial Growth Factor, abbreviated as VEGF, represents a protein signaling molecule which plays a crucial role in both vasculogenesis and angiogenesis.
There are five different types of VEGF – VEGF-A, VEGF-B, VEGF-C, VEGF-D, and placental growth factor (PlGF).
VEGF-A, sometimes referred to as VEGF, was discovered in the 1980s by various groups of researchers. VEGF-A is a single gene, but it is one of the VEGF proteins which exists in sub-types; this occurs due to the way its messenger RNA (mRNA) is processed, and in the case of VEGF-A this gives rise to nine sub-types.
This protein is a “mitogen”, necessary for the survival of vascular endothelial cells. VEGF-A, expressed in many organs and tissues, also allows plasma and proteins contained within the plasma to pass through the endothelial layer of blood vessels without damaging the vessel. Mice lacking VEGF-A do not survive, and exhibit abnormal vasculature; therefore, it is likely that VEGF-A is essential for the formation of blood vessels at early stages of embryonic development.
VEGF-B is also one gene that exists as two protein sub-types – VEGF-B167 has 167 amino acids, while VEGF-B186 has 186 amino acids. VEGF-B167 is the more common sub-type, and it binds to heparan sulfate. On the other hand, VEGF-B186 is a secreted protein which is able to diffuse in vivo, unlike VEGF-B167. While the role of VEGF-B is not clear, studies have shown that it is expressed during embryonic development, and studies using mice without VEFG-B showed abnormal heart function – indicating that it is essential for heart function.
VEGF-C can act as a signal in its unprocessed and processed forms, which helps to form and maintain the lymphatic system. The unprocessed form undergoes a complex processing method before it becomes the mature VEGF-C. VEGF-C is highly expressed in the heart, ovaries, placenta, skeletal muscles and small intestine in adult humans, while lower levels of VEGF-C are seen in the kidneys, lungs, pancreas, prostate, spleen and testes. Studies on mice lacking VEGF-C have shown that they are not viable, therefore VEGF-C is most likely to be an essential growth factor. Other studies have shown that VEGF-C is expressed in regions of the mouse embryo where lymphatic vessels sprout to form embryonic veins.
VEGF-D is produced in an unprocessed form, and like VEGF-C has to undergo a complex processing before maturation. It is highly expressed in lung tissue, both during embryonic development and in adults. VEGF-D is also highly expressed in the heart, lungs, skeletal muscles, colon and small intestine, while lower levels of VEGF-D are seen in the ovaries, testes, prostate, spleen and pancreas. Unlike VEGF-C negative mice, mice lacking VEGF-D are viable; hence, it is possible that functions of VEGF-D can be performed by other growth factors.
PlGF is another member of the VEGF family with multiple sub-types. As the name implies, it is mainly expressed in the placenta, but it is also expressed in the heart, skeletal muscles, skin and retina; interestingly, mice lacking PlGF show reduced vascularization in the retina of their eyes, suggesting the possibility that PlGF is important in the development of vasculature in the eyes. It should also be noted that PlGF enhances VEGF signaling.
There is another VEGF, VEGF-E, which is a factor produced by a virus. VEGF-E causes new blood vessels to develop at the sight of parapoxvirus infection. VEGF-E also has the ability to make blood vessels more permeable, akin to VEGF-A.
How is VEGF production triggered?
Studies have shown that various growth factors and hormones can lead to the production of VEGF. Examples include tissue growth factor-β, epidermal growth factor and platelet-derived growth factor BB; platelet-derived growth factor was shown to induce VEGF-A production from wounds, which encourage healing.
Cytokines – including tumor necrosis factor- α (TNF-α) – have also been shown to induce VEGF expression. TNF-α is a pro-inflammatory cytokine, and it influences angiogenesis by inducing the release of molecules which, in turn, induce angiogenesis (such as VEGF-A and VEGF-C).
An example of a hormone which induces VEGF expression is estrogen. It has been shown that estrogens not only enhance transcription of VEGF-A, but also make VEGF-A mRNA more stable, meaning that more VEGF-A protein would be translated.
Furthermore, hypoxia (or a lack of oxygen) induces the expression of certain genes, such as VEGF. Genes which are activated by hypoxia have what is termed a “hypoxia response element”, and in VEGF-A this element resides in the promoter region of the gene. These hypoxia response elements act as binding sites for “hypoxia induced factor”, or HIF, which is a protein complex that acts as a transcription factor made of HIF-1α and HIF-1β. The aforementioned heterodimer is stabilized by hypoxia because it leads to a decrease in HIF1-α prolyl and asparaginly hydroxylation. This subsequently leads to HIF being able to act as a transcription factor, and enhancing the expression of genes including VEGF-A, VEGF-C and PlGF.
How does VEGF stimulate the growth of new blood vessels?
VEGF contains a signal sequence which is cleaved as VEGF is made. There are three protein-tyrosine kinase receptors for VEGF – VEGFR1, VEGFR2 and VEGFR3. Some of the VEGF proteins are also able to bind to heparan sulfate glycans, which are found on the plasma membrane, as well as in the extracellular matrix.
VEGFR1, found on endothelial cells, binds VEGF-A, VEGF-B and PlGF, and its activation leads to different results depending on the stage of development and location of the receptor. VEGFR1 binds more strongly to VEGF-A when compared to VEGFR2, but its tyrosine kinase activity is weaker compared to VEGFR2. The activation of VEGFR1 does not directly lead to proliferation; however, it does lead to increased expression of the urokinase type of plasminogen activator, as well as plasminogen activator inhibitor-1 from endothelial cells; these are involved in the degradation of the extracellular matrix and cell migration.
VEGFR2 binds smaller sub-types of VEGF-A, mature VEGF-C, mature VEGF-D and VEGF-E. Signaling from this receptor is the primary way in which endothelial cell migration, proliferation and survival is mediated, and it is also responsible for increased vascular permeability. Studies have shown that VEGFR2 is essential for proper development of the vascular system, as animal studies have shown that embryos lacking VEGFR2 are not viable, and show that differentiation of endothelial cells or blood vessel formation have not occurred. Activation of VEGFR2 leads to the production of platelet-activating factor from endothelial cells, and this acts to promote cell division and migration as well as increasing vascular permeability.
VEGFR3 binds VEGF-C and VEGF-D, and is found in lymphatic endothelial cells. Activation of VEGFR3 has been shown to lead to its association with Shc and adaptor protein. Signaling from VEGFR3 has been shown to play a role in angiogenesis and lymphangiongenesis (i.e. the formation of lymph vessels) in adults, as well as being important for the remodeling of the primary capillary plexus in the embryo.
What are the normal roles of VEGF?
As mentioned above, VEGF plays a role in the development of vessels during embryonic development. Studies have shown that a concentration gradient of VEGF is required for the development of the cardiovascular system, and its decrease leads to potentially lethal underdevelopment of the cardiovascular system. VEGF receptors are also critical for proper angiogenesis, and defects can also lead to lethal abnormalities.
In adults, angiogenesis not only maintains blood and lymph vessels, but is also involved in would healing and female reproductive cycle. Therefore, its stimulation can be beneficial in various indications (such as peripheral arterial disease and ischemic heart disease).
Wounds lead to the activation of platelet, which initiates the blood clotting cascade to stop the bleed. This also leads to the release of growth factors and cytokines, including VEGF-A, subsequently resulting in the recruitment of neutrophils and monocytes to the wound site via signaling from VEGFR1. This then leads to production of other cytokines, which together with platelet-derived TGF-β and other serum factors induce expression of VEGF-A from the keratinocytes at the wound site.
Studies have shown that VEGF-A plays a role in the female reproductive cycle, both in the ovaries and the endometrium, the lining of the womb. Luteinizing Hormone (LH) seems to the key regulator of angiogenesis in the ovaries, while estrogen and progesterone seems to influence VEGF-A expression in the endometrium.
What roles does VEGF play in cancer?
Studies have shown that VEGF is expressed in a wide variety of cancers – including breast cancer, colorectal cancer, small-cell lung cancer, non-Hodgkin’s lymphoma, cervical cancer, prostate cancer and thyroid cancer. There has been research into using VEGF inhibitors as a potential treatment options, and it has been shown that it is possible that VEGF inhibitors can stop tumor growth and metastasis.
Angiogenesis is necessary for tumor progression, and studies have revealed that tumor cells produce VEGF and the surrounding endothelial cells show increased expression of VEGF receptors. VEGF induces the formation of vesiculo-vascular organelles, which forms a support matrix that allows the growth of tumor and endothelial cells, as well as the invasion of stromal cells into the tumor. This support matrix can further develop into a tumoral stroma; this somewhat resembles the wound healing process, and while the processes involved are not exactly the same, there are striking similarities.
Sources
- Roskoski, R. Jr (2007). Vascular endothelial growth factor (VEGF) signaling in tumor progression. Critical Reviews in Oncology/Hematology http://www.brimr.org/Reprints/135.pdf
- Hoeben, A. et al. (2004). Vascular Endothelial Growth Factor and Angiogenesis. Pharmacological Reviews http://pharmrev.aspetjournals.org/content/56/4/549.abstract
- Neufeld, G. et al. (1999). Vascular endothelial growth factor (VEGF) and its receptors. The FASEB Journal https://www.fasebj.org/doi/abs/10.1096/fasebj.13.1.9
Further Reading
- All VEGF Content
- What is VEGF?
- VEGF Classification
- VEGF Mechanism
- VEGF Production
Last Updated: Aug 13, 2019

Written by
Dr. Maho Yokoyama
Dr. Maho Yokoyama is a researcher and science writer. She was awarded her Ph.D. from the University of Bath, UK, following a thesis in the field of Microbiology, where she applied functional genomics toStaphylococcus aureus . During her doctoral studies, Maho collaborated with other academics on several papers and even published some of her own work in peer-reviewed scientific journals. She also presented her work at academic conferences around the world.
Source: Read Full Article
