
No one disputes that the world is unfair. But no one expected a vaccine gap between the global rich and poor that was this bad, this far into the pandemic.
Inequity is everywhere: Inoculations go begging in the United States while Haiti, a short plane ride away, received its first delivery July 15 after months of promises—500,000 doses for a population over 11 million. Canada has procured more than 10 doses for every resident; Sierra Leone’s vaccination rate just cracked 1% on June 20.
It’s like a famine in which “the richest guys grab the baker,” said Strive Masiyiwa, the African Union’s envoy for vaccine acquisition.
In fact, European and American officials deeply involved in bankrolling and distributing the vaccines against coronavirus have told The Associated Press there was no thought of how to handle the situation globally. Instead, they jostled for their own domestic use.
But there are more specific reasons why vaccines have and have not reached the haves and have-nots.
COVID-19 unexpectedly devastated wealthy countries first—and some of them were among the few places that make the vaccines. Export restrictions kept the doses within their borders.
There was a global purchase plan to provide vaccines for poorer countries, but it was so flawed and underfunded that it couldn’t compete in the cutthroat competition to buy. Intellectual property rights vied with global public health for priority. Rich countries expanded vaccinations to younger and younger people, ignored the repeated pleas of health officials to donate their doses instead and debated booster shots – – even as poor countries couldn’t vaccinate the most susceptible.

The disparity was in some ways inevitable; wealthy nations expected a return on their investment of taxpayer money. But the scale of the inequity, the stockpiling of unused vaccines, the lack of a viable global plan to solve a global problem has shocked health officials, though it wasn’t the first time.
“This was a deliberate global architecture of unfairness,” Masiyiwa told a Milkin Institute conference.
“We have no access to vaccines either as donations or available for us to purchase. Am I surprised? No, because this is where we were with the HIV pandemic. Eight years after therapeutics were available in the West, we did not receive them and we lost 10 million people.”
“It’s simple math,” he said. “We have no access. We have no vaccine miracle.”
___
The World Health Organization has duly updated its epidemic playbook after every outbreak, most recently with Ebola in mind. Then, as often in the decades before, an emerging illness was largely contained to countries lacking robust public health services, with poor sanitation and crowded living conditions and limited travel connections.
For years, the WHO assessed countries’ readiness for a flu pandemic: The United States, European countries and even India ranked near the top. The U.S. readiness was 96%, and Britain at 93%.

On Jan. 30, 2020, WHO declared the coronavirus outbreak in China to be a global emergency. It would be months before the word “pandemic” became official.
But that same day, the Coalition for Epidemic Preparedness and Innovations, or CEPI, was planning for the worst. CEPI announced “a call for proven vaccine technologies applicable for large scale manufacturing,” according to minutes from its scientific advisory group. CEPI said it would be critical “to support the strategy for global access” early in the game.
CEPI quickly invested in two promising coronavirus vaccines being developed by Moderna and CureVac.
“We said very early on that it would be important to have a platform where all countries could draw vaccines from, where there’s accountability and transparency,” said Christian Happi, a professor at Nigeria’s Redeemer’s University and a member of CEPI’s scientific advisory committee. “But the whole idea was that we thought rich countries would fund it for the developing world.”
Happi said officials never expected the pandemic would strike first and hardest in Europe and the U.S. Or that their assessment of preparedness in the world’s most advanced economies would prove horrifically optimistic.
Global health experts would soon come to realize that rich countries “could sign a piece of paper saying they believe in equity, but as soon as the chips are down, they will do whatever they want,” he said.
On March 16, five days after the global pandemic was declared, the novel mRNA vaccine developed by Moderna was injected into a trial participant for the first time.

By then, the disease was tearing through the elderly populations of Europe and the United States.
Moderna and Pfizer/BioNTech were the first companies to come out with an mRNA vaccine, devising methods of mass production almost on the fly. Scientists at Britain’s Oxford University also came up with a vaccine with a more traditional platform, and Bill Gates brokered a deal for them to partner with AstraZeneca, a pharmaceutical company with global reach but no experience in vaccine production.
On April 30, the deal was confirmed: AstraZeneca took sole responsibility for the global production and distribution of the Oxford vaccine and pledged to sell it for “a few dollars a dose.” Over the next few weeks, the U.S. and Britain secured agreements totaling 400 million doses from AstraZeneca.
The race to make and secure vaccines was on, and the United States and Britain were leagues in front of the rest of the world—a lead they wouldn’t lose. Still, both countries would see life expectancy decline by at least a year in 2020, the biggest drop since World War II. In the European Union, 22 countries saw their average lifespans cut short, with Italy leading the list.
___
But as grim as the situation was, all those countries had a major advantage: They were home to the pharmaceutical companies with the most promising vaccine candidates, the world’s most advanced production facilities, and the money to fund both.
On May 15, 2020, President Donald Trump announced Operation Warp Speed and promised to deliver vaccines against coronavirus by New Year’s. With unparalleled money and ambition behind the project, Warp Speed head Moncef Slaoui was more confident than his counterparts in Europe that a vaccine was in the offing. He signed contracts almost without regard to price or conditions.

“We were frankly focused on getting this as fast as humanly possible. If I had to redo it, I probably should have voiced more of a global dimension,” said Slaoui. “The operation had focused, which was frankly also part of its success, on staying out of the politics and making the vaccines.”
The idea of including clauses to ensure that vaccines would go to anyone besides Americans wasn’t even considered.
At the same time, the U.S. repeatedly invoked the Defense Production Act—18 times under the Trump Administration and at least once under Biden. The moves barred exports of crucial raw materials as factories were ramping up production of the as-yet-unapproved vaccines—and eventually, of the vaccines themselves.
But it also meant those materials would run low in much of the rest of the world. The U.S. stranglehold would lift only in spring 2021, and only partially.
Operation Warp Speed supercharged the global race to secure vaccines, but it would still take another two weeks until COVAX—the COVID-19 Vaccines Global Access Facility—was formally announced as the entity to ensure equity, with the Serum Institute of India as the core supplier for the developing world.
COVAX had the backing of the World Health Organization, CEPI, vaccines alliance Gavi and the powerful Gates Foundation. What it did not have was cash, and without cash it could secure no contracts.
“Operation Warp Speed signed the first public deals and that started a chain reaction,” said Gian Gandhi, UNICEF’s COVAX coordinator for supply. “It was a like a rush on the banks, but to buy up the expected supply.”

Some involved in the COVAX project flagged India as a potential problem early on, according to minutes of meetings in late spring and early summer of 2020.
India’s government had blocked exports of protective gear, but many global health authorities who hadn’t fully grasped the extent of pandemic nationalism found it unimaginable that the country would block vaccines when the world was counting on them. Also, India had so far been spared the waves of death that were sweeping across Europe and the Americas.
A separate plan put forward by the government of Costa Rica and the World Health Organization to create a technology-sharing platform to expand vaccine production foundered. Not a single company agreed to share its blueprints, even for a fee—and no government pushed them behind the scenes, according to multiple people involved in the project.
On the global scale, the one organization that could have pushed for more technology sharing was the Gates Foundation, whose money to WHO nearly matches that of the U.S. government.
Instead, Bill Gates defended stringent intellectual property rights as the best way to speed innovation. His foundation poured money and influence into the Access to COVID-19 Tools Accelerator, which also failed to generate the money or influence needed to ramp up production outside already existing hubs.
In the United States, meanwhile, manufacturing and the trials went on in parallel, which is where taxpayers and the companies took enormous risks that paid off for both.
But in retrospect, Slaoui said, given the sheer amount of taxpayer money involved, each time they signed new contracts the U.S. and other countries could have pushed companies harder to share their knowledge, if only for the duration of the pandemic.

“From a geopolitical standpoint, it’s critical that they do that,” he said.
Nowhere was the situation more dire than Africa. In February, WHO’s African expert in vaccine development, Richard Mihigo, was among many who said the continent’s experience with other pandemics had uniquely prepared it for a complex vaccine deployment.
Five months later, contemplating the plight of a continent that gets 99% of its vaccines from abroad, Mihigo adds a rueful footnote: “One of the lessons we learned from this pandemic is how badly prepared we were in vaccine production in the region and how dependent we were on imports.”
Those imports have only barely begun to materialize—and they are insufficient to meet even the limited goals of the COVAX initiative to vaccinate at least 20% of the population of 92 low- and middle-income countries by the end of this year.
___
From the start, the coalition of organizations that created COVAX found themselves fighting the last war.
The plan was designed as an international pool to spur demand for vaccines and treatment of diseases with a relatively small global footprint, said Winnie Byanyima, head of UNAIDS.

Something like Ebola. But the coronavirus pandemic looked nothing like an Ebola outbreak.
“That itself was a structural weakness,” she said.
Although the World Bank and the International Monetary Fund had between them set aside billions for vaccinating the developing world, that money was intended to go to countries and was out of bounds for a global vaccine sharing plan like COVAX, said Mike Muldoon, managing director for innovative finance at the Rockefeller Foundation.
Meanwhile, governments competed to secure contracts for vaccines by the hundreds of millions.
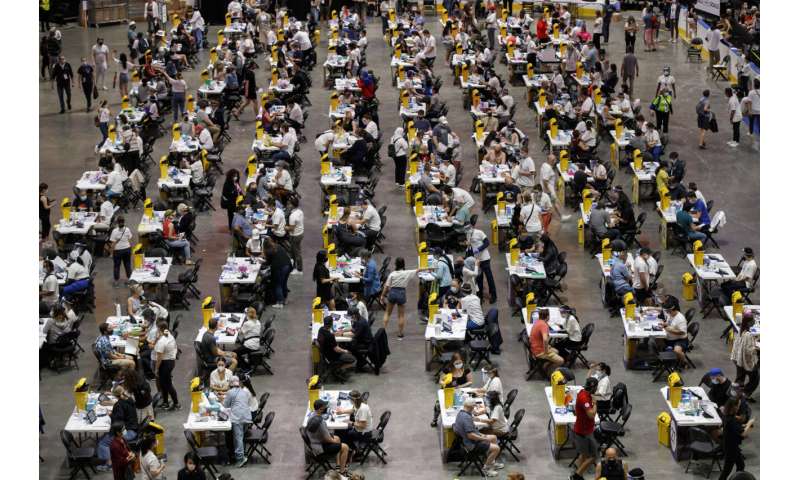
On Dec. 8, Britain became the first country to formally authorize a start to widespread vaccinations, injecting 90-year-old Margaret Keenan with a dose of the Pfizer-BioNTech vaccine. Six days later, the United States started its own vaccinations. And on Dec. 26, the EU followed suit. China and Russia had been vaccinating even before releasing data from their homegrown inoculations.
The Western companies with the most promising doses, including Pfizer/BioNTech, Moderna and AstraZeneca, had by then been churning out vials for months before formal approval, based on pledges from the wealthy countries that an enormous market awaited. Those doses were stockpiled in Europe and North America and a small number of countries, like Israel, that paid a premium.
COVAX pleaded for cash to do the same. Instead, it got pledges.

“As time passed and it became clear which vaccine candidates were going to be the leading contenders and which were most likely to succeed, the governments that had resources went and bought the supplies,” CEPI chief executive Dr. Richard Hatchett told the AP. “COVAX was not in a position to do that.”
Months later, when COVAX finally had the money to sign deals for global supplies, Hatchett acknowledged they were at the end of the line.
The lack of capital available to vaccine makers to boost their capacity outside the small number of existing manufacturing hubs was also “a lost opportunity,” Hatchett said.
“We approached the international financing institutions, including the World Bank and the (International Finance Corporation) about making those investments and they were not willing to do that,” he said. CEPI ended up investing about $1.5 billion, far less than what a major financial institution might have been able to commit.
COVAX missed its own goal of beginning vaccinations in poor countries at the same time as rich ones. It finally delivered vaccines on Feb. 24, to Ghana, a load of 600,000 AstraZeneca doses manufactured by the Serum Institute of India and transported by UNICEF planes.
By that date, 27% of the population in Britain had been vaccinated, 13% in the U.S., 5% in Europe—and 0.23% in Africa, in countries that had secured their own bilateral deals after growing impatient with COVAX delays. The rift was growing by millions of doses every day.
And pharmaceutical plants were beginning to crumble under the promises they’d made.
AstraZeneca announced repeated delivery cuts to Europe. Pfizer’s production briefly slowed. A fire at a Serum Institute construction site prompted a letter to Brazil warning that “supply to you cannot be guaranteed in the foreseeable months.” Moderna supply cuts soon followed to Britain and Canada.
In the United States, officials tossed millions of corrupted doses of vaccine from the Emergent Biosolutions plant in Baltimore after discovering that workers had inadvertently blended ingredients from the AstraZeneca and Johnson & Johnson vaccines. An untold number of doses were never produced because of new restrictions meant to prevent errors. Many of those vaccines were intended for export.
So COVAX had to hope that the AstraZeneca vaccine being produced in India would come through, because it had secured few of the innovative mRNA doses that are now considered the most effective against the coronavirus variants. The initial refrigeration requirements were daunting, and the price was higher than the traditional vaccine candidates.
The mRNA vaccines are widely considered a scientific and manufacturing triumph—and a risky bet. Never before approved for use against any disease, they are now considered a hugely promising medical innovation and a potential gamechanger against infection.
But by the time it was clear the mRNA doses were a viable alternative, even in poor countries with limited cold chain, the available supply had been snapped up in Europe, the United States and Canada. And India, in the throes of its own COVID-19 surge, diverted its vaccines for its own use.
According to the People’s Vaccine Alliance, a grouping of human rights organizations advocating for broader sharing of vaccines and their underlying technology, the coronavirus has created nine new billionaires. The top six are linked to the successful mRNA vaccines.
For Byanyima, of UNAIDS, this is a travesty and a sign that the world has learned little in the decades since the AIDS pandemic was brought under control in the United States, only to kill millions in Africa because treatments were unaffordable: “Medicines should be a global public good, not just like a luxury handbag you buy on the market.”

COVAX has delivered only 107 million doses, and now is forced to rely upon uncertain donations from countries that may prefer to donate directly to the needy, so they can receive the credit.
A readout from its June board meeting slipped in an acknowledgement that it needed to better interpret and respond to market conditions and “the reality that a higher risk appetite is needed in a pandemic setting.”
___
For the pharmaceutical industry, mRNA is the ultimate confirmation that hard work and risk-taking is rewarded. And those companies keep tight hold on the keys to their successful vaccines.
When Moderna and Pfizer created new production lines, it was in the insular European and American manufacturing networks that had as much stake as anyone in both ensuring that the injections meet the highest standards and keeping promises not to abuse intellectual property.
Many public health officials have pushed for technology transfer during the pandemic. Initially resistant, the Gates Foundation has changed its position in favor of sharing.
Dr. Clemence Auer, the EU’s lead negotiator for vaccine contracts last summer, said the question of compelling pharmaceutical companies to suspend their vaccine intellectual property rights to increase the worldwide supply of coronavirus vaccines never even came up.
“We had a mandate to buy vaccines, not to talk about intellectual property, ” Auer said.
“The global community should have had this discussion back in 2020 but that didn’t happen,” he said. “Maybe we should have done it last year, but now it’s too late. It is spilled milk.”
CEPI includes equity clauses in the vaccines that it invests in, among them the successful Moderna candidate, but has yet to invoke them during the pandemic. Some include requirements to make a vaccine available to populations in need at affordable prices, as is the case in CEPI’s Moderna contract. But Moderna was first available exclusively in wealthy countries and even now only limited amounts are going outside Europe and the United States.
A separate push to lift intellectual property restrictions on vaccines and medicines has also gone nowhere in the World Trade Organization.
And WHO is reticent to make demands of donor nations or the pharmaceutical companies. It needs them for other aspects global health—and for its own continued existence. The Biden administration has reversed Trump’s decision to defund and leave WHO, but the damage has been done.
“A lot of these multinational organizations, these plans, these coalitions, they don’t have teeth to enforce what they think is a fair and equitable way to distribute resources,” said Dr. Ingrid Katz, an infectious disease researcher at the Center for Global Health at Massachusetts General Hospital. She said the key question is whether vaccines and essential medications are a commodity or a right.
“If it’s going to be a commodity, we’re going to keep walking down this road every time we have something like this,” she said.

And if it is all going to rely on the generosity of rich countries, a lot of people are going to die. Four million have died already.
In all, at the recent Group of Seven meeting of wealthy nations pledged to donate 850 million doses, compared with the 11 billion that WHO says will be needed to end the pandemic.
A close look at the G-7 promises of donations shows that most aren’t expected to be delivered until well into 2022. The Biden administration fell short on its pledge to send 80 million doses abroad by the end of June: By mid-July, at least 44 million doses had been sent, including 2.5 million to Canada, which has already given at least one vaccine dose to more of its population than any other country. Africa has yet to receive its doses from the United States.
___
Oceans away from the deprivation of the developing world, 7-year-old Russell Bright and his 5-year-old brother went to Ochsner Medical Center in New Orleans to get their shots—part of a trial for young children. Maybe they got the vaccine; maybe they got the placebo.
Wearing a Spider-Man mask, Russell said he longs for a vacation trip to the water park and then a return to school without having to wear masks and stay at arms’ length from his friends.
“Both me and my wife are already vaccinated,” said his father, Adam, “and so the sooner I can get them vaccinated and to feel comfortable being outside, not having to wear a mask, I thought the easiest way to get it is to go through the trial.”



Scientists agree that children are at low risk from COVID-19. But that hasn’t stopped richer countries from stockpiling precious vaccine supplies to inoculate the young, even as poor countries have few or no shots to give.
A recent meeting of WHO’s vaccine allocation group disbanded with nothing accomplished, because there was no vaccine to allocate. “Zero doses of AstraZeneca vaccine, zero doses of Pfizer vaccine, zero doses of J&J vaccine,” said Dr. Bruce Aylward, a senior advisor at the organization.
“Every single one of our suppliers is unable to supply during this period because others are making demands on those products, others who are vaccinating very young populations that are not at risk,” Aylward said.
Both Trump and Biden administration officials reject the notion that the U.S. or any country would share vaccines until they’d protected their own. And they both note that the U.S. bore the brunt of the pandemic last year, topping the world in confirmed cases and deaths.
“We had a responsibility to what I say, ‘put on our own oxygen masks before helping others,'” CDC Director Rachelle Walensky said in May.
But a plummeting jet takes all passengers with it, whether or not they are wearing masks. And the failure to provide vaccines across the globe ensures that COVID-19 will continue to spread, and mutate, and sicken, and kill.
Source: Read Full Article
