Placentas can provide critical information about the health of the mother and baby, but only 20 percent of placentas are assessed by pathology exams after delivery in the U.S. The cost, time and expertise required to analyze them are prohibitive.
Now, a team of researchers has developed a novel solution that could produce accurate, automated and near-immediate placental diagnostic reports through computerized photographic image analysis. Their research could allow all placentas to be examined, reduce the number of normal placentas sent for full pathological examination and create a less resource-intensive path to analysis for research—all of which may positively benefit health outcomes for mothers and babies.
“The placenta drives everything to do with the pregnancy for the mom and baby, but we’re missing placental data on 95 percent of births globally,” said Alison Gernand, assistant professor of nutritional sciences in Penn State’s College of Health and Human Development. “Creating a more efficient process that requires fewer resources will allow us to gather more comprehensive data to examine how placentas are linked to maternal and fetal health outcomes, and it will help us to examine placentas without special equipment and in minutes rather than days.”
The team’s study was presented at the International Federation of Placenta Associations meeting held in Buenos Aires, Argentina, in September and at the International Conference on Medical Image Computing and Computer Assisted Intervention held in Shenzen, China, in October.
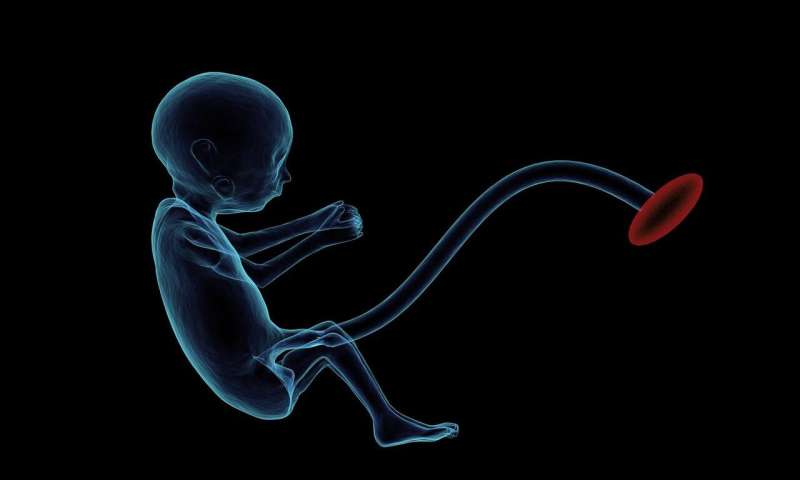
The patent-pending technology uses artificial intelligence to analyze an image of each side of the placenta after delivery and then produces a report with critical information that could impact the clinical care of the mother and child, such as whether the fetus was getting enough oxygen in the womb or if there is a risk of infection or bleeding.
Currently, there are no evidence-based standards to determine when a placenta should be examined, and low-income countries and areas where home births are more prevalent often lack resources to conduct even a baseline placental analysis. This digital tool could offer a solution, as an individual would need only a smartphone or tablet with the appropriate software.
“Even in very low-resource areas, someone typically has a smartphone,” explained Gernand. “Our goal is for a medical professional or trained birth attendant to take a photo which, after analysis through licensed software, could provide immediate information that aids in the care of the mother and baby.”
For example, an umbilical cord with an abnormal insertion point or excessive twisting can be a predictor of neonatal stroke. Examination after a stillbirth could give a family information about whether future stillbirths may reoccur and help medical professionals advise them on possible interventions.
To create the system, the researchers analyzed 13,000 high-quality images of placentas and their corresponding pathology reports from Northwestern Memorial Hospital. Then, the researchers labeled a training set of images with data points critical to understanding the placenta, such as areas of incompleteness and the umbilical cord insertion point.
The images were used to train neural networks using CPU and GPU servers that could automatically analyze new placental images to detect features linked to abnormalities and potential health risks. Their system produced predictions on unlabeled images efficiently, and comparisons with the original pathology reports demonstrated the system’s high accuracy and clinical potential.
“Past analyses have typically examined features independently and used a limited number of images,” said James Wang, professor in Penn State’s College of Information Sciences and Technology. “Our tool leverages artificial intelligence and a large and comprehensive dataset to make multiple decisions at the same time by treating the different parts of the placenta as complimentary. To our knowledge, this is the first system for comprehensive, automated placental analysis.”
Additionally, this tool could advance pregnancy research and be useful for long-term care by providing clinically meaningful information to patients and practitioners.
Said Wang, “We don’t want to replace pathologists, but rather we want to provide physicians with more information right at birth so they can make an efficient and informed decision about how to care for the mother and child.”
Source: Read Full Article
