To date, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has claimed the lives of more than 5.6 million people worldwide. The pandemic has been one of the most significant risks to the global economy and society in modern times.

Study: Aerosol measurement identifies SARS-CoV 2 PCR positive adults compared with healthy controls. Image Credit: Aliaksandra Post/Shutterstock.com
Droplets and aerosols are the primary routes of transmission for SARS-CoV-2. Therefore, aerosol measurements may be used to identify highly contagious individuals ("super spreaders" or "super emitters") and distinguish between SARS-CoV-2 infected and non-infected individuals.
In a new study, exhaled aerosols were compared between infected SARS-CoV-2 patients and healthy controls for the first time. A preprint version of this study, which is yet to undergo peer review, is available on the medRxiv* server.
Aerosols are described as a suspension of solid or liquid particles in a gas mixture (such as air), whereas droplets are defined as particles larger than 100 μm. Small aerosol particles can be detected in the exhaled air during regular breathing. During conversation, laughter, or singing, larger particles of various sizes and compositions are expelled more frequently.
According to a recent study out of Singapore, 85% of SARS-CoV-2 viruses were found in a tiny fraction of inhaled aerosols. The spread of viruses and bacteria via aerosols has been studied before, for example, in Mycobacterium tuberculosis, influenza viruses, and respiratory syncytial viruses (RSV). Aerosols have been identified as a critical element in the spread of associated diseases.
From February to June 2021, scientists from various institutions conducted prospective observational cohort research at the Goethe University Hospital in Frankfurt to assess inhaled aerosol concentration and particle size in SARS-CoV-2 PCR-positive and -negative people. Adults (18–99 years old) who had a SARS-CoV-2 PCR test were eligible within 48 hours of the aerosol measurement.
The study
Exhaled particle counts >5,000/L were judged extremely high, implying that contagiousness might be elevated in a viral infection situation. No participants in the SARS-CoV-2 PCR-negative group had very high exhaled particle counts, whereas 15.6% of the SARS-CoV-2 PCR-positive group had very high counts, accounting for 64.8% of total exhaled particle counts in the group. Furthermore, 15.6% was responsible for 51.2% of all inhaled particles, amounting to 3.5% of all patients.
There were no significant changes in aerosol concentration due to sex, BMI, or smoking status; however, there was a modest rise in aerosol concentration with increasing age. There was a minor difference in median exhaled particle counts between the three subgroups of respiratory failure, pneumonia, and immunocompromised individuals when solely examining the SARS-CoV-2 PCR-positive group.
In terms of particle size distribution, the available size channels (14 in total, ranging from 0.15 to 5.0 µm) were divided into three size bands: 0.3 µm, 0.3–0.5 µm, and >0.5–5.0 µm. The majority of the aerosols were identified in the smallest range in both groups (>90% in the SARS-CoV-2 PCR-positive group and >78% in the -negative group). Increases in total aerosol concentration were dominated by increases in particles 0.3 µm, especially in the positive group.
A receiver operating characteristic (ROC) analysis was performed to assess the accuracy of the exhaled particle count as a diagnostic for detecting SARSCoV-2 PCR-positive infection. With an area under the curve (AUC) of 0.8918 and an exhaled particle count cut-off value of 596/L, the test's sensitivity was 79.7% and specificity was 85.7%.
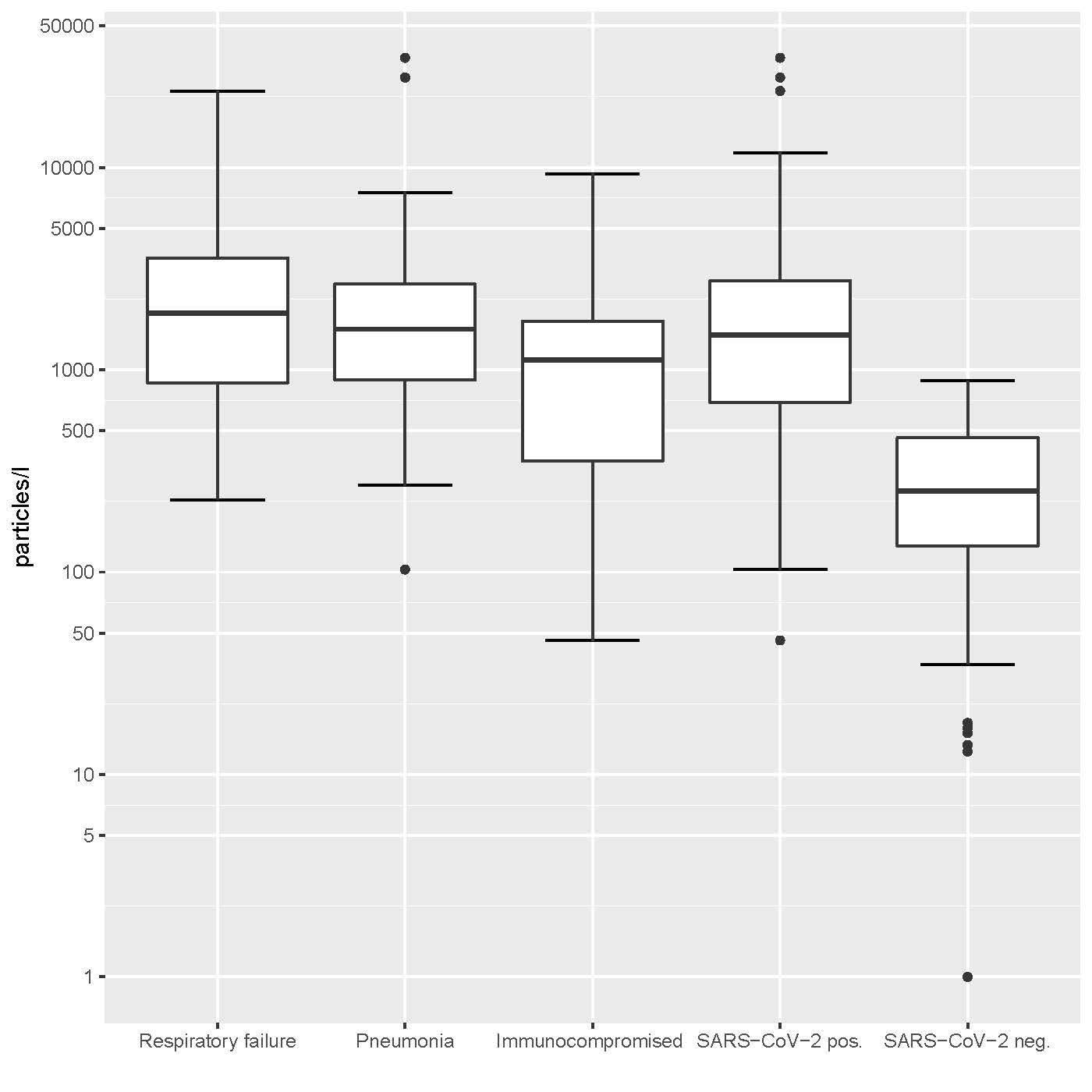
Aerosol particle counts in SARS-CoV-2 PCR-positive and -negative patients.
Implications
Exhaled aerosol particle concentrations differed considerably between SARS-CoV-2 PCR-positive and -negative individuals. Because these aerosol particles originate at the lung's base, infected alveolar epithelial cells type 2 may create more surfactant, resulting in more tiny droplets to convey the virus out of the lung. Improved control of SARS-CoV-2 transmission could result from a better understanding of respiratory aerosol production. In addition, portable aerosol measurement devices could be a valuable tool in the future for detecting possibly contagious individuals using a non-invasive breath test.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Aerosol measurement identifies SARS-CoV 2 PCR positive adults compared with healthy controls, Desireé Gutmann, Gerhard Scheuch, Timon Lehmkühler, Laura-Sabine Herrlich et al, medRxiv, 2022.01.21, https://doi.org/10.1101/2022.01.21.22269423, https://www.medrxiv.org/content/10.1101/2022.01.21.22269423v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Bacteria, Breathing, Coronavirus, Coronavirus Disease COVID-19, Diagnostic, Hospital, Influenza, Pandemic, Particle Size, Pneumonia, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Singing, Smoking, Syndrome, Tuberculosis, Virus
.jpg)
Written by
Colin Lightfoot
Colin graduated from the University of Chester with a B.Sc. in Biomedical Science in 2020. Since completing his undergraduate degree, he worked for NHS England as an Associate Practitioner, responsible for testing inpatients for COVID-19 on admission.
Source: Read Full Article
