Rising numbers of liver cancer in Aboriginal and Torres Strait Islander communities has led experts at Flinders University to call for more programs, including mobile liver clinics and ultrasound in rural and remote Australia.
The Australian study, just published in EClinicalMedicine, reveals the survival difference was largely accounted for by factors other than Indigenous status—including rurality, comorbidity burden and lack of curative therapy.
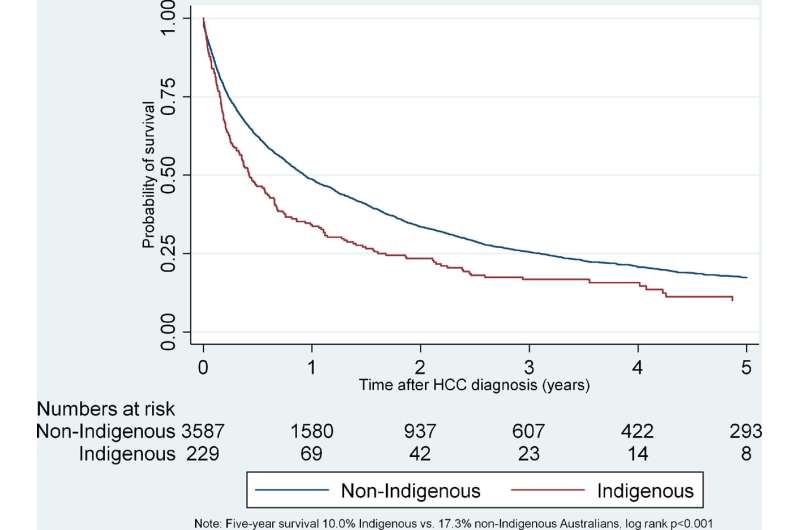
The study of liver cancer, or hepatocellular carcinoma (HCC), included 229 Indigenous and 3587 non-Indigenous HCC cases in South Australia, Queensland and the Northern Territory.
“The major finding was important differences in cofactors for HCC between Indigenous and non-Indigenous patients, with Indigenous patients more frequently having multiple cofactors for HCC such as hepatitis B, diabetes and alcohol misuse,” says Flinders University Professor Alan Wigg, who led the investigation.
While cancer care is difficult to deliver to remote Australia, he says HCC is preventable with surveillance.
“What is needed is a culturally appropriate model of care in rural communities that screens for liver disease and identifies at-risk patients,” says Professor Wigg, who also is head of the Hepatology and Liver Transplant Medicine Unit at the Southern Adelaide Local Health Network in South Australia.
“At-risk patients need regular six-monthly high-quality liver ultrasound surveillance, which supports a model of care involving mobile liver clinics using fibro-scans and liver ultrasound.”
This latest research confirms both the incidence and mortality are about 2.6 fold higher in Indigenous compared to non-Indigenous Australians.
Liver disease and HCC is the sixth most common cause of death and HCC is the second most common cause of cancer death in Indigenous Australians.
Other important associations with HCC in Indigenous Australians included a higher comorbidity burden, lower socioeconomic status, younger age at onset, higher proportion of females and poorer five-year survival rates.
“Our study shows the majority of HCC cases in Indigenous Australians occurred in patients living outside of metropolitan areas, to help address the problem of liver disease and HCC and to design effective interventions to reduce the morbidity and mortality from these diseases,” says co-author Professor Patricia Valery, who leads the QIMR Berghofer Medical Research Institute’s Cancer and Chronic Disease research group.
“This suggests that lower access to care may be contributing to poorer survival in these patients.
“The study findings highlight that there is still more work to do on interventions to reduce Indigenous mortality from liver disease and HCC,” she says.
Source: Read Full Article
