An international team of scientists led by Mass Eye and Ear, a member of Mass General Brigham, and Boston Children’s Hospital, has discovered a new genetic mutation that may be a root cause of severe cases of childhood glaucoma, a devastating condition that runs in families and can rob children of their vision by 3 years of age.
Through advanced genome-sequencing technology, the researchers found a mutation in the thrombospondin-1 (THBS1) gene in three ethnically and geographically diverse families with childhood glaucoma histories. The researchers then confirmed their findings in a mouse model that possessed the genetic mutation and went on to develop symptoms of glaucoma driven by a previously unknown disease mechanism.
The new findings, published December 1 in the Journal of Clinical Investigation, could lead to improved screening for childhood glaucoma and earlier and more targeted treatments to prevent vision loss in children with the mutation, according to the study’s authors.
“This is a very exciting finding for families affected by childhood glaucoma,” said Janey L. Wiggs, MD, Ph.D., Associate Chief of Ophthalmology Clinical Research at Mass Eye and Ear and the Vice Chair for Ophthalmology Clinical Research and Paul Austin Chandler Professor of Ophthalmology at Harvard Medical School.
“With this new knowledge, we can offer genetic testing to identify children in a family who may be at risk for the disease and start disease surveillance and conventional treatments earlier to preserve their vision. In the future, we would look to develop new therapies to target this genetic mutation.”
Leading cause of childhood blindness
Childhood, or congenital, glaucoma is a rare but serious disease that presents in children as early as birth and as late as 3 years of age. Despite its rarity, childhood glaucoma is responsible for 5 percent of cases of child blindness worldwide.
Glaucoma causes irreversible damage to the eye’s optic nerve, often due to buildup of pressure inside the eye (intraocular pressure, or IOP). In adults, this damage can occur over time without symptoms, which is why the disease is often referred to as a “sneak thief of sight.”
Children and babies with childhood glaucoma, however, can be born with severe disease and vision loss or lose their vision later in childhood due to elevated IOP. This increase in pressure not only damages the optic nerve but can also affect other structures in a child’s eye like the cornea. Children with childhood glaucoma typically require surgeries as early as the first three to six months of life, followed by several more operations throughout their childhood.
With childhood glaucoma, there is typically a strong hereditary component often with multiple members of a family affected by the condition. According to Dr. Wiggs, by better understanding the genes involved, genetic testing can give affected families peace of mind to learn whether their child might be at risk for developing the disease.
Uncovering the genetic underpinnings of disease
For decades, researchers have turned towards genetics to better understand the cause of glaucoma. When Dr. Wiggs first began this line of research 30 years ago, scientists were only able to identify regions of the genome affected in glaucoma.
Thanks to advances in genomic technology, researchers gained the ability to review the complete genetic makeup of individuals with and without glaucoma to determine which specific genetic mutations play a role in the disease. Research led by Dr. Wiggs in 2021 used a dataset of more than 34,000 adults with glaucoma to identify 127 genes associated with the condition.
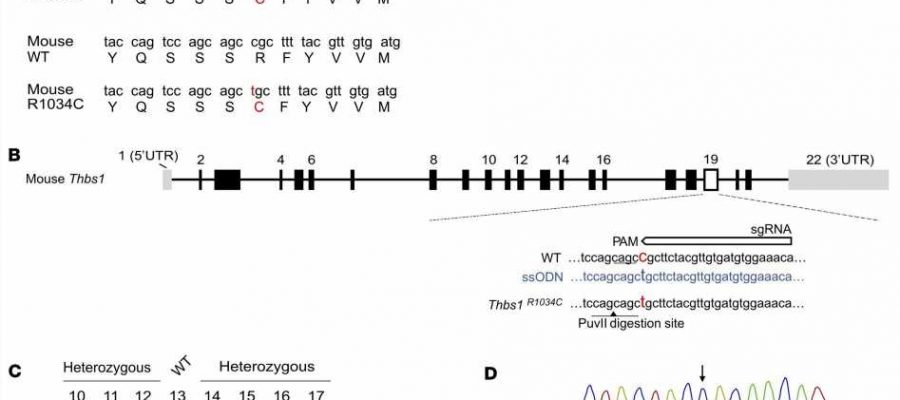
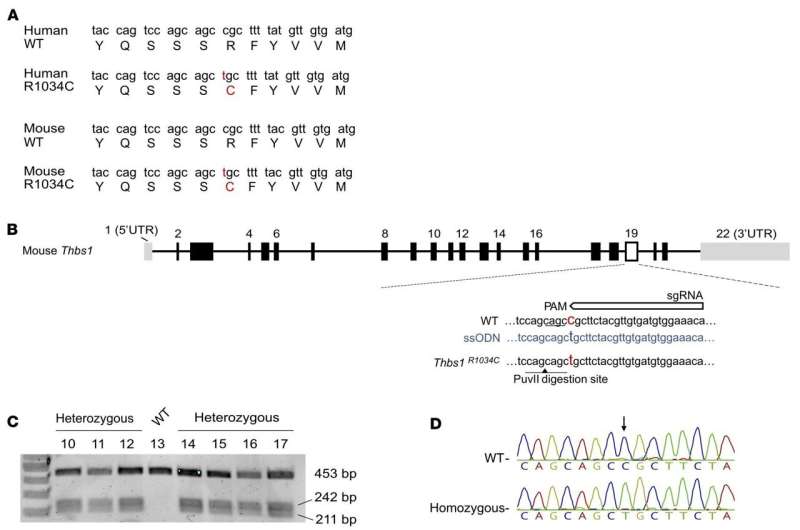
To better study the genetic mutations in childhood glaucoma, Dr. Wiggs and her Mass Eye and Ear team first looked at exome sequences from an American family of European-Caucasian descent who had been part of an earlier research project and found a striking and novel variant in thrombospondin-1, a well-known protein in the body involved in a number of important biological processes, such as the formation of new vessels (angiogenesis) and tissues.
This mutated gene was not found in people without childhood glaucoma, nor in large population genetic databases. The amino acid altered by the mutation was evolutionarily conserved, indicating an important role in the protein function. This finding led Dr. Wiggs to connect with colleagues at Flinders University in Australia to see if they had any childhood glaucoma families with thrombospondin mutations.
They surprisingly found two families with an alteration at the same amino acid: one of mixed European and Indian descent, and one Sudanese family originally from Africa.
“What was really striking about this finding is that these families all possessed this genetic variant, and it was not possible for them to be related because they were from such diverse backgrounds,” said Dr. Wiggs. “That meant there was something really important about this mutation.”
To further test this hypothesis, the researchers collaborated with Robert J. D’Amato, MD, Ph.D., the Judah Folkman Chair in Surgery in the Vascular Biology Program at Boston Children’s Hospital, and a professor of Ophthalmology at Harvard Medical School. Dr. D’Amato’s team developed a mouse model with the THBS1 mutation and found that the mouse also had features of glaucoma.
“Thrombospondin-1 is well known as a potent inhibitor of blood vessel growth, or angiogenesis,” said Dr. D’Amato, who has studied angiogenesis for more than three decades. “I assumed at first that THBS1 mutations were disrupting blood vessel formation in the eye, but our animal models showed normal angiogenesis. We realized that there must be another mechanism.”
Specifically, D’Amato’s lab showed that the mutation caused abnormal thrombospondin proteins to accumulate in the intraocular drainage structures of the eye involved with regulating IOP, which in turn, led to a buildup of pressure that damaged the optic nerve and led to the loss of retinal ganglion cells, thereby causing vision loss.
This was the first time that researchers identified this kind of disease mechanism for causing childhood glaucoma.
“This work highlights the power of international collaborations,” said study co-author Owen M. Siggs MD, DPhil, associate professor at Flinders University and the Garvan Institute of Medical Research in Australia. “There’s such incredible genetic diversity across the globe, and comparing this information is becoming more and more critical for discoveries like this.”
Personalizing care for families with future study
The new study has significant clinical implications, according to the researchers. While more work remains before comprehensive genetic testing can be offered, every gene that is found presents another opportunity to be able to identify causative mutations in these families through screening, according to the authors.
Therapeutically, knowledge of this gene mutation can lead to earlier treatments with conventional therapies. For example, if a baby is born with this mutation, their eye care specialist can better inform the parents of the risks and develop an appropriate disease-monitoring and treatment plan.
Identifying this new mechanism and gene at the root of childhood glaucoma could also lead to new therapies that would target the accumulation of abnormal proteins. The researchers also aim to determine if other THBS1 mutations are involved in adult-onset disease, like primary open-angle glaucoma, or milder forms of the disease if the mutation is not as pronounced.
The researchers will also continue to look for new genes associated with childhood glaucoma in the hopes of one day developing very comprehensive screening.
“Dr. Wiggs is an international expert in glaucoma genetics and has worked tirelessly to unravel the genetic contributions to these blinding diseases. These findings provide important insights into the causes of childhood glaucoma and offer the prospect of targeted therapy,” said Joan W. Miller, MD, Chair of Ophthalmology at Mass Eye and Ear and Massachusetts General Hospital, Ophthalmologist-in-Chief at Brigham and Women’s Hospital, and Chair of Ophthalmology and the David Glendenning Cogan Professor of Ophthalmology at Harvard Medical School.
“The collaboration is a powerful demonstration of the strength of bedside-to-bench-to-bedside translational research, in uncovering disease pathogenesis and developing therapies for patients.”
More information:
Haojie Fu et al, Thrombospondin 1 missense alleles induce extracellular matrix protein aggregation and TM dysfunction in congenital glaucoma, Journal of Clinical Investigation (2022). DOI: 10.1172/JCI156967
Journal information:
Journal of Clinical Investigation
Source: Read Full Article