Interactions between the developing heart and lungs are essential for proper growth and maturation; however, much is still unknown about the co-development of these critical organs. To provide fresh insight, a team of collaborators from CMU and Boston University recently presented the first laboratory model for human heart and lung co-development to help researchers discover new strategies to probe the underlying mechanisms of cardio-pulmonary interactions.
Organs begin to take shape during the first few months of life as the baby grows as an embryo inside the womb. During this embryogenesis, different layers of stem cells are activated to turn into specific types of cells, for example, a heart or lung cell. The heart and lungs develop from two distinct germ layers within the embryo, the mesoderm and endoderm, which must communicate with each other for the organs to form correctly.
“My scientific training is rooted in developmental biology,” explained Charlie Ren, assistant professor of biomedical engineering. “I was curious about how we could borrow learnings from embryogenesis to achieve a deeper understanding of when something goes wrong with our critical organs, like what we see in congenital diseases. Animal models offer some answers, but there are key differences that prevent us from really translating data for human understanding. We set out to generate a model that could be directly applied to human health.”
In work published in eLife, the group developed a human model of heart and lung co-development during embryogenesis using lab-grown human induced pluripotent stem cells (hiPSCs). The hiPSCs were treated with chemical signals, causing them to form different germ layers that developed into early forms of heart and lung cells. Then, the cells were transferred into a tailored growing condition, where they arranged into three-dimensional structures termed microtissues.
https://youtube.com/watch?v=ZDWVih7zVCQ%3Fcolor%3Dwhite
Interestingly, the research revealed that lung cells matured faster when grown in microtissues accompanied with developing heart cells, when compared to developing lung cells alone.
“Traditionally in a lab setting, we’ve developed organs separately, to curb technical barriers related to balancing the lineage of two organs and a recipe that was needed to support both of them,” noted Ren. “However, through this novel co-development model, we found that the lung needs the heart. We’ve been able to show that when the heart develops with a lung and provides beneficial factors, the lung will mature better and faster. Currently we are studying the underlying molecular mechanisms of this intriguing phenomenon.”
“This is a truly exciting model of heart and lung co-development that provides important insight not only into embryogenesis, but also presents new strategies for bioengineering replacement heart and lung tissue for therapeutic applications,” added Adam Feinberg, professor of biomedical engineering and materials science and engineering, and a co-author on the study.
https://youtube.com/watch?v=n27sV_a6obw%3Fcolor%3Dwhite
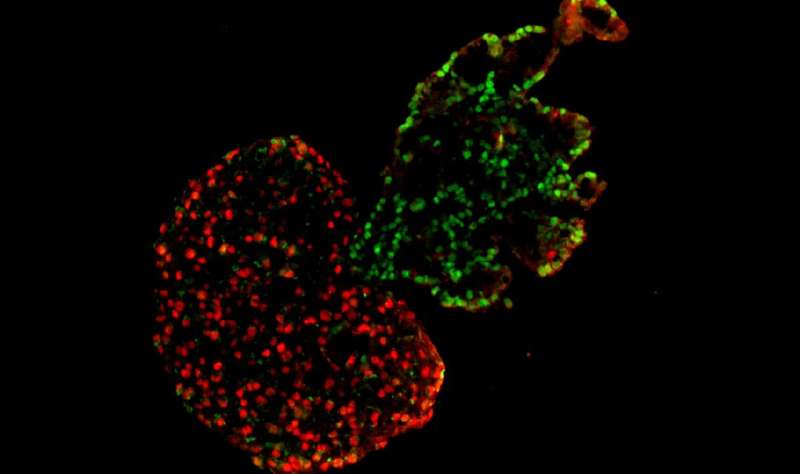
The model also demonstrated that co-developing heart and lung tissues automatically separate from each other during later stages, establishing an accurate boundary between the two neighboring organs.
“Though this work, we named a new term: cardiopulmonary tissue segregation,” said Ren. “We observed that the cells seem to have some sort of intelligence to know their ‘closer’ friend; the lung cells automatically came together without leaving one cell behind, and the heart cells did the same. As they developed, they moved away from each other and separated. It’s almost magic.”
Source: Read Full Article
