The immune system is equipped with numerous cell types that effectively fight the various pathogens, humans can encounter during their lives. T cells, for example, have a receptor through which they can specifically recognize and bind antigens. However, in recent decades, cell types with similar protective properties have been discovered that do not possess a specific antigen receptor.
Only a few years ago, scientists identified a group of lymphocytes, so-called ‘innate lymphoid cells’ (ILCs), which are now among the most important players in the body’s immune defense and make a significant contribution to the fight against pathogens. Unlike T cells, ILCs do not patrol the bloodstream but are predominantly tissue-resident cells. ILCs reside in various tissues where they interact with many immune and non-immune cell types and contribute to immune surveillance, activation of inflammatory responses, tissue homeostasis and repair and barrier functions. They are found in the bone marrow, secondary lymphoid organs such as lymph nodes and, most prominently, in non-lymphoid tissues with mucosal barriers such as the lung or the small intestine.
The ambivalent role of ILC2 in immune defense
The size of the ILC population and the subset composition varies between organs and can undergo dynamic changes during immune challenge. Type II ILCs (ILC2s) are the dominant subtype in the lung and have been shown to play a major role in immune defense against parasitic worm infection or in wound healing. On the other hand, ILC2s also contribute to the pathology of allergic respiratory inflammation such as asthma.
As in other tissues, ILC2s in the lung expand and differentiate during the first weeks of life after which a fraction persists as tissue-resident cells during adulthood. However, ILC2s can be generated and recruited from other tissues also during adult life in normal physiology and inflammatory conditions. It was unclear whether these ILC2s have specialized functions or whether they were recruited to replenish the local pool of resident cells.
Single-cell atlas of lung innate lymphoid cells
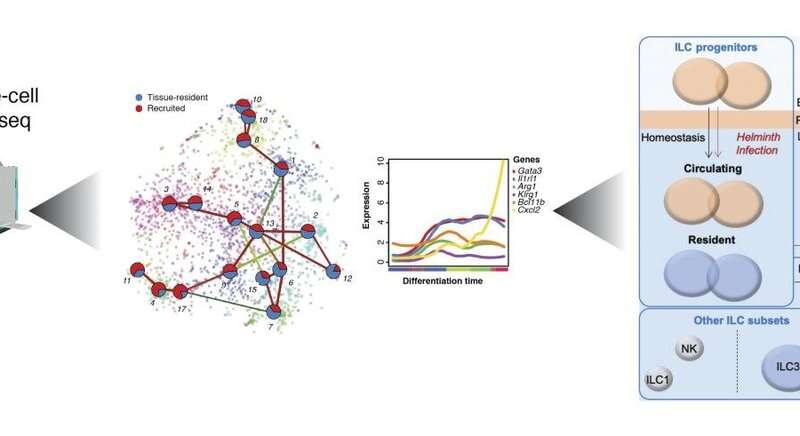
To shed light on these unknown mechanisms, scientists at the Max Planck Institute of Immunobiology and Epigenetics in Freiburg, headed by Dominic Grün, and colleagues from the Würzburg Institute of Systems Immunology led by Georg Gasteiger teamed up with researchers from New York and Marseille to generate a comprehensive single-cell atlas of mouse ILC populations in the bone marrow, neonatal and adult lung during normal physiological condition and during worm infection.
They discovered a pool of local progenitors which receives influx from the bone marrow and has the potential to generate the full spectrum of mature ILC2s observed in the lung during worm infection.
Cell plasticity in response to changing tissues
“Our work sheds light on how the local population of ILC2s in the lung is maintained. We found that progenitors recruited to the lung from other tissues via the bloodstream adjust to the lung environment by modulating their gene expression and differentiate into mature ILC2s that are almost indistinguishable from their counterparts derived from lung-resident progenitors. This is an exciting example for the plasticity of immune cell states in response to changing tissue environments,” says Dominic Grün, Max Planck group leader and member of the CIBSS—Centre for Integrative Biological Signalling Studies, Cluster of Excellence at the University of Freiburg.
The study published in the scientific journal Immunity describes a “continuum” of ILC2 differentiation stages connecting the progenitors with the mature populations, including previously unknown ILC2 subtypes.
“We were able to reveal the complexity of the functions of ILC2s in an unprecedented manner and at the same time draw conclusions about their origin and development,” explains Patrice Zeis, first author of the study. To detect the heterogeneity and development of lung ILC2s in a comparable systemic way, the scientists combined single-cell RNA sequencing with machine learning approaches. Thus, they successfully created “molecular fingerprints” for thousands of innate immune cells in the murine lung, and derived novel insights on the cell’s identity, functions and the developmental relationships between the cells in the model organism.
Source: Read Full Article
