A team of researchers from Illinois Institute of Technology and the University of Washington is trying to change the way that the field of biology understands how muscles contract.
In a paper published on January 25, 2023, in the Proceedings of the National Academy of Sciences titled “Structural OFF/ON Transition of Myosin in Related Porcine Myocardium Predict Calcium Activated Force,” Illinois Tech Research Assistant Professor Weikang Ma and Professor of Biology and Physics Thomas Irving—working in collaboration with Professor of Bioengineering Michael Regnier’s group at Washington—make the case for a second, newly discovered aspect to muscle contraction that could play a significant role in developing treatments for inherited cardiac conditions.
The consensus for how muscle contraction occurs has been that the relationship between the thin and thick filaments that comprise muscle tissue was a more straightforward process. When targets on thin filaments were activated, it was thought that the myosin motor proteins that make up the thick filaments would automatically find their way to those thin filaments to start generating force and contract the muscle.
“No, no, no: the motor proteins have to be woke up and released before they can do that,” says Irving. “There’s both a release, but there’s also an attraction. We thought if you release them, they zip off and find their targets. They’re actually sucked in… Once they get close enough, they’re electrostatically attracted and they’re more likely to bind, sort of like a tractor beam at the end.”
By better understanding this relationship between the thick and thin filaments in regards to muscle contraction, genetic conditions that have gone untreated until now may eventually have medical remedies. The diseases can range from dilated cardiomyopathy—where the heart muscle is too weak and ultimately struggles to pump blood throughout the body—to hypertrophic cardiomyopathy, where the muscle works too hard and eventually becomes thickened, potentially reducing blood flow.
“Until recently, there weren’t any drugs; now, they’re starting to emerge,” adds Irving. “What we want to do is to make sure that we fix the right problem. We need to understand this process.”
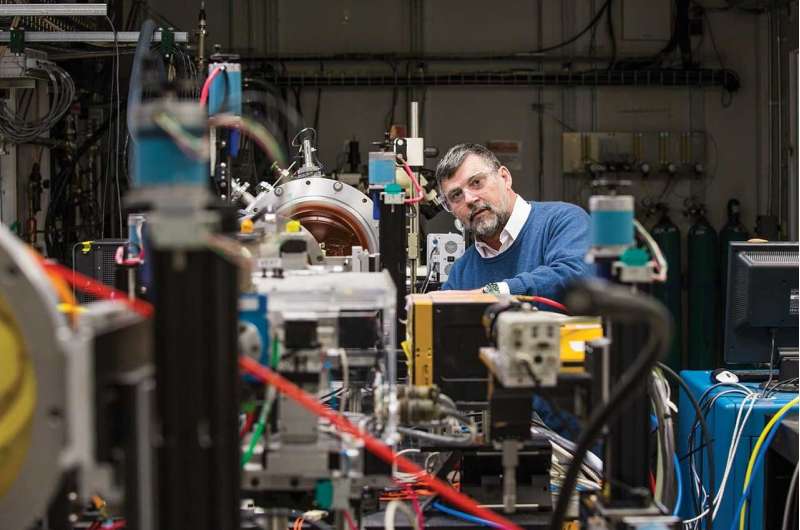
Part of what has allowed the team to make its case is the information that it gathered using a state-of-the-art technique called small-angle X-ray diffraction, a technique that Irving has been perfecting as part of the Biophysics Collaborative Access Team (BioCAT) in partnership with groups such as the National Institutes of Health and Argonne National Laboratory since the 1990s. This technique allows researchers to gather data in a way that Irving says is more accurate than other techniques currently being used.
“In electron microscopy, you can’t see motion, it’s a static measurement. You can’t do a time result,” says Irving. “In our case, we can take movies; we can do a physiological experiment and see these molecules moving in real physiological time. That’s what’s so special about it.”
“That was another important point that we were making here: You really, really do want to do these X-ray experiments to see what’s actually happening with these myosin heads moving because you can see them, rather than only indirectly surmising what’s going on,” Irving adds.
While Irving is excited about potential treatment for these diseases, the search for understanding remains his biggest motivation.
“I just want to know how things work,” says Irving. “If it helps people, all the better.”
More information:
Weikang Ma et al, Structural OFF/ON transitions of myosin in relaxed porcine myocardium predict calcium-activated force, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2207615120
Journal information:
Proceedings of the National Academy of Sciences
Source: Read Full Article
