The heart is an electromechanical organ whose functioning can be captured in the form of electrical voltage pulses, calcium ion waves, and mechanical contractions. Inherited conditions, stress, drugs, or aging can lead to disruption of any of these waves and put a person’s life at risk. Cardiac electrophysiology and electromechanics study how such waves function and what can keep them stable and safe.
Bioengineers have recently adopted human-induced pluripotent stem-cell-derived cardiomyocytes (hiPSC-CMs) as a model of the human heart. Such “lab-on-a-chip” human hearts can be used to study the disruption in these cardiac waves in response to various stimuli, using patient’s own reprogrammed cells. Optical imaging can help visualize the waves, however highly sensitive high-speed cameras are needed for this purpose, and each one of them can be expensive, costing around $100,000 in US dollars.
Against this backdrop, researchers directed by Emilia Entcheva at The George Washington University, have now developed a portable and low-cost macroscopic mapping system for all-optical cardiac electrophysiology. Instead of using electrical stimuli, they triggered voltage, calcium waves, and mechanical contractions in hiPSC-CMs using light (optogenetic stimulation).
“Optogenetics uses light-sensitive proteins from algae that are genetically expressed in human cells to control them in a manner similar to that realized using electrical impulses. The utilization of light, however, enables the stimulation of many samples simultaneously in a contactless manner without any wiring. This is not possible with electrical impulses,” explains Entcheva. Their work was published recently in the Journal of Biomedical Optics.
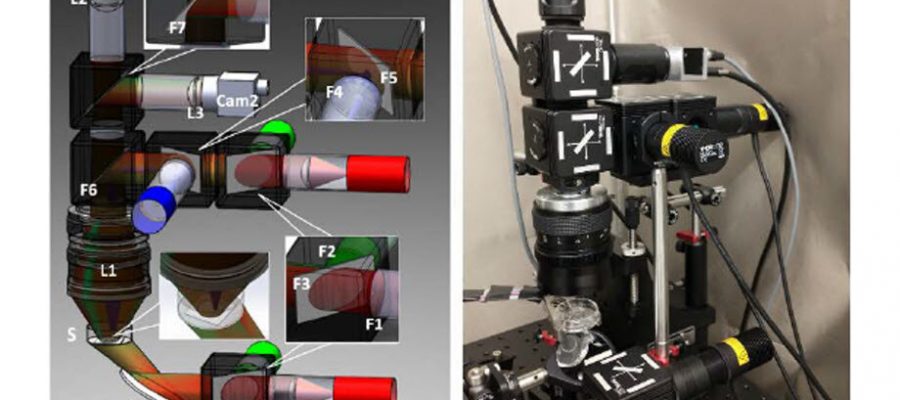
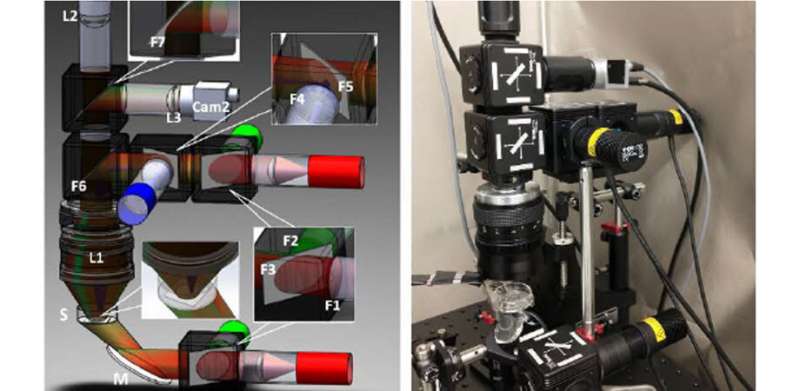
To make their system affordable, the researchers used inexpensive high-speed machine vision CMOS cameras, priced 100 times lower than the scientific CMOS cameras typically used for this purpose. Yuli Heinson, postdoc in the lab and first author, built a multicamera system, utilizing LEDs and off-the-shelf components for stimulation and control.
Using oblique LED illumination made it possible to discern local dye-free signals for small mechanical contractions, while imaging centimeter-scale area. “It likely represents an interference-based detection mechanism,” says Entcheva. The whole reconfigurable multicamera setup cost less than $15,000, had a small form factor, i.e., was smaller than conventional designs, and was portable.
Once the system was in place, the researchers extensively quantified the effects of different experimental conditions on the measured wave parameters. Using illumination at various powers, they showed that the electrical and optogenetic stimulations of hiPSC-CMs were equivalent.
However, because calcium waves were imaged using green light-excitable fluorescent sensors, and such light may partially also activate the blue light-based optogenetic actuators, the researchers found that extremely low illumination needed to be used to not alter calcium wave velocity. Voltage and calcium maps provided similar information under controlled electrical or optogenetic pacing conditions. The velocity of these waves varied with temperature and the type of experimental solution used.
Lastly, the researchers presented potential applications of their system. The system was shown to detect conduction changes due to drugs targeting cell–cell coupling. In addition, its transillumination mode could be reconfigured into an epi-illumination setting for imaging thicker samples, such as cardiac image slices or the surface of whole hearts.
The advantages of the novel all-optical setup are not restricted to the above demonstrations. The combination of multiple optical sensors and actuators in the setup design can handle spectral congestion and avoid parameter distortion. The new technology can help characterize hiPSC-CMs and further basic and translational cardiac arrhythmias studies, work that Julie Han, co-author on the paper, is pursuing during her doctoral studies. Moreover, it can open doors to other practical medical science applications in the near future.
“Patient-derived cells enable personalized testing of the most suitable drug combination. Therefore, the developed technology can help decide the best treatment for a patient, promoting effective and safe cures,” says Entcheva.
“Further, any drug development undergoes preclinical cardiotoxicity safety testing. The presented inexpensive system can help devise better and faster assays that can save lives and money. Its compactness can allow deployment in large pharma-linked labs as well as lower-resource settings, such as academic labs and developing countries,” she concludes.
More information:
Yuli W. Heinson et al, Portable low-cost macroscopic mapping system for all-optical cardiac electrophysiology, Journal of Biomedical Optics (2023). DOI: 10.1117/1.JBO.28.1.016001
Journal information:
Journal of Biomedical Optics
Source: Read Full Article